The use of x-ray contrast media in patients with kidney impairment can result in higher rates of long-term adverse events such as death, heart attack, and stroke, and different contrast agents can have varying adverse event rates, according to a study published online today in the Clinical Journal of the American Society of Nephrology.
Nearly a third of patients who received contrast media during x-ray coronary angiography studies experienced adverse events after the exams, and patients with signs of contrast-induced nephropathy (CIN) had higher adverse event rates than those without CIN, according to a research team led by Dr. Richard Solomon, who is with Fletcher Allen Health Care and is also section chief of the division of nephrology at the University of Vermont in Burlington.
What's more, the study found that patients receiving a low-osmolar agent, iopamidol (Isovue, Bracco, Princeton, NJ), had lower rates of CIN and adverse events compared to those who received an iso-osmolar agent, iodixanol (Visipaque, GE Healthcare, Chalfont St. Giles, U.K.).
CARE update
The new study is an update of the Cardiac Angiography in Renally Impaired Patients (CARE) study, which was published in Circulation in 2007. The original CARE study examined CIN rates in a population of 414 patients with moderate to severe renal impairment who had received iopamidol and iodixanol during coronary angiography. The primary end point of the prospective, randomized, multicenter study was the development of contrast-induced nephropathy, comparing CIN development rates shortly after patients received contrast.
While the study was useful in identifying the relationship between CIN and contrast administration, the problem is that the commonly used techniques to detect CIN do not actually measure kidney damage, but rather kidney function, according to Solomon. One could reasonably assume that reduced kidney function meant kidney damage had occurred, but there was no empirical data to prove the assumption.
The new CARE study set out to answer this question by following the original patient population over the course of a year to track long-term adverse event rates, ranging from less serious events such as revascularization or other therapy to major events such as death, heart attack, stroke, or the development of end-stage renal disease requiring dialysis.
The researchers then compared adverse event rates in this population to rates of CIN that had been recorded shortly after contrast was administered. CIN was defined according to several commonly used measures of kidney function such as serum creatinine (SCr) or cystatin C levels. The researchers also compared adverse event rates between the two groups of patients who were randomized to receive either iopamidol or iodixanol.
Some 120 patients from the original group were lost to follow-up, leaving Solomon and colleagues with 294 patients for the current study. Data were collected from July 2006 to February 2008. The group analyzed the data using several different definitions of CIN, but found the most accurate measures to be either a SCr increase of ≥ 0.3 mg/dL or a cystatin C increase of ≥ 15%. All of the 294 patients had SCr measurements, but only 242 had cystatin C data.
Solomon et al found that a total of 31% of patients (92 of 294) had adverse events, with 13% (n = 38) classified as major events (death, heart attack, stroke, or end-stage renal disease). More importantly, the rate of adverse events was higher in the patients defined as having CIN. Using the definition of CIN as a SCr increase of ≥ 0.3 mg/dL, the group found that 43% of patients in the CIN group (22 of 51 patients) had adverse events of all kinds, versus 29% (70 of 243 patients) in the non-CIN group.
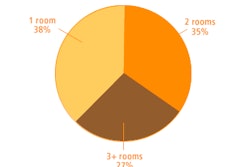
Adverse events by CIN definition
|
Using other criteria to define CIN also revealed a relationship: With CIN defined as a cystatin C increase of ≥ 15%, 42% of patients who had CIN (25 of 60 patients) later experienced adverse events, versus 26% of patients who did not have CIN (47 of 182 patients).
Solomon believes that the study indicates that measures of CIN like SCr and cystatin C levels can be used to predict long-term outcomes.
"We found that the arm with [lower CIN rates] had fewer adverse outcomes," Solomon told AuntMinnie.com. "This suggests that kidney injury has an impact on adverse event rates. If you prevent the kidney injury, it lowers adverse event rates."
Contrast agent wars
The second major finding of the study -- the difference in adverse events between iopamidol and iodixanol -- will probably become ammunition in the ongoing war between contrast manufacturers over product safety. Vendors have been trading barbs over whose agent has the better safety profile since the publication of the Nephrotoxic Effects in High-Risk Patients Undergoing Angiography (NEPHRIC) study in 2003. (The CARE study was supported by funding from Bracco, and Solomon is a consultant to the company -- see sidebar.)
In the current CARE study, Solomon and colleagues found that of the 92 CIN patients who experienced both major and less serious adverse events, 27% (n = 39) had received iopamidol, versus 36% (n = 53) in the iodixanol group. For only major events, the difference was not as strong, with major adverse events occurring in 11% of iopamidol patients (n = 16) versus 15% of iodixanol patients (n = 22). There was no difference in adverse events between the contrast agents in the subgroup of patients who did not experience CIN.
Adverse events by contrast medium and adverse event type
|
The current findings differ somewhat from the original CARE study. Iopamidol had lower CIN rates than iodixanol in the 2007 research, but the difference was not statistically significant when using SCr levels to define CIN, Solomon said. But in the current study, when researchers used the definition of CIN as an increase in cystatin C levels of ≥ 15%, they found a statistically significant difference between the products with respect to adverse event rates.
|
Contrast firms duel over research claims Clinical research doesn't usually end up as evidence in a court of law, but most of the time research doesn't involve the fiercely competitive contrast media market. Bracco and GE locked legal horns in a lawsuit over the 2003 NEPHRIC study, which compared the safety profile of two GE agents, Visipaque and Omnipaque. Bracco pointed out that the study involved only the two GE products, but in marketing materials GE claimed that Visipaque was safer than other products that were not included in the research, including Bracco's Isovue. A federal judge in March 2009 ruled in Bracco's favor on those assertions, ordering GE to pay $11.4 million in damages. Solomon's work was raised in the lawsuit as the court reviewed various clinical studies on contrast safety, including the 2007 CARE study. Court documents note that Bracco paid Solomon consulting fees as part of its effort to counter damage from the NEPHRIC study, which resulted in Visipaque gaining market share at the expense of Isovue. Solomon received $30,000 from Bracco for publication of a review article published in Investigative Radiology in August 2006 (Vol. 41:8, pp. 651-660), while a co-author on the CARE study, Dr. Samin Sharma of Mt. Sinai Medical Center in New York City, received $50,000 for his costs associated with an article published in Catheterization and Cardiovascular Interventions in July 2005 (Vol. 65:3, pp. 386-393), according to court documents. The judge overseeing the case, U.S. District Court Judge Freda Wolfson, found that the Sharma and Solomon articles were "biased" and "methodologically flawed," and that "no reasonable conclusions on the relative nephrotoxicity of Visipaque, Omnipaque, and Isovue" could be drawn from the studies. Her opinion did not extend to the CARE study. Bracco representatives dismissed the assertion that Solomon and others would alter their findings based on consulting fees, and pointed out that the CARE paper is a multicenter study involving a number of investigators. "Dr. Solomon was one of many authors on that paper, and was not the only one that performed the study," said Dr. Alberto Spinazzi, senior vice president of medical and regulatory affairs worldwide for Bracco. "It was a team effort of many investigators," and it's inappropriate to raise questions about their motives, he added. In her legal opinion settling the Bracco/GE lawsuit, Wolfson concluded by expressing exasperation at the extent of commercial ties to clinical research in the contrast media market. "Bracco and [GE Healthcare] are the primary players in the field of [contrast media] and, thus, fiercely compete against each other in the marketplace, obviously target each other, and look to tout their own products whenever possible," the judge's ruling said. "It appears to be commonplace, if not a necessary part of the industry, for companies to spend significant amounts of capital in support of scientific comparative studies to promote sales of their products." "Moreover, the Court was surprised by the revelations that virtually every clinical trial, study, and resultant publication in this area was sponsored by [GE Healthcare] or Bracco. In some cases, the principal investigators were paid consultants to one of these companies. This has led the Court to conclude, and lament, that there is little in the way of a truly independent clinical study in the [contrast media] market." |
Solomon believes that in addition to statistical significance, the new study has clinical significance as well.
"I think [the results] are strong enough to recommend using iopamidol rather than iodixanol," Solomon said. "When you take into account iopamidol's lower cost, better kidney safety profile, and higher iodine content, which results in potentially better images, it's the preferred agent."
But those conclusions are disputed by GE, which objects to the methodology used in the new study. In particular, GE points out that the 2007 CARE study didn't find a statistically significant difference in CIN between the agents, but in the 2009 study, Solomon et al did find a difference after applying a new criteria for CIN -- a cystatin C increase of ≥ 15% -- that wasn't used in the original trial and that isn't clinically accepted, according to Dr. Eric Cantor, head of medical and professional affairs at GE.
"The [2007] CARE trial did not show a statistically significant difference between iopamidol and Visipaque," Cantor said. "Yet in order to drive some data that would be significant, the authors utilized a new and unproven post-hoc definition of CIN ... that is by no means standard and leads to a conclusion that I believe cannot be supported."
For his part, Solomon said such criticism missed the main point of the research, which is the relationship of acute kidney injury to long-term clinical outcomes, rather than a comparison of two competing products.
"The fact that it involved two different agents is irrelevant to the paper," Solomon said. "It's not the purpose of the paper. We would have written the paper if iodixanol came out on top of iopamidol. The message would not have changed."
In an independent commentary on the CARE study's results, Dr. Joseph Schoepf of the Medical University of South Carolina in Charleston said the study fills in a missing link in research on contrast media reactions by following patients over the long term.
"This is the first study I've seen that goes beyond a short-term follow-up in kidney function," Schoepf said. "As such, I think the study is valid statement."
But Schoepf issued a cautionary note on the study's findings regarding the safety profiles of iopamidol versus iodixanol. For one, the study population consists of patients who are already very sick, with high event rates. For another, the patient population may not be large enough to demonstrate major differences.
"With a population of 294, to say someone died because they got contrast agent A or contrast agent B would be very difficult to establish," Schoepf said. "You would need to have a larger patient group to establish that connection."
By Brian Casey
AuntMinnie.com staff writer
June 25, 2009
Related Reading
Sodium bicarbonate helps avoid contrast nephropathy, June 5, 2009
Court orders GE to pay Bracco, correct Visipaque ads, March 30, 2009
Atrial natriuretic peptide protects against contrast nephropathy, March 27, 2009
Iso-osmolar contrast does not lower the nephrotoxicity rate in CKD patients, October 27, 2008
Intra-arterial safer than intravenous administration of contrast medium, October 16, 2008
Copyright © 2009 AuntMinnie.com