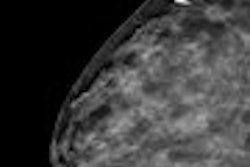
A new study published online this week found that computer-aided detection (CAD) improves the sensitivity of mammography screening with only a small boost in the patient recall rate. The research offers a rebuttal to last year's New England Journal of Medicine study that found that CAD actually reduced the accuracy of breast screening centers that used it.
Since the introduction of CAD technology, the question of whether CAD for mammography screening helps or hurts has been a point of controversy. Last year's NEJM study associated CAD with reduced accuracy of interpretations of screening mammograms, casting aspersions on the technology's effectiveness and provoking panic among clinicians and CAD developers as third-party insurers threatened to cut reimbursement.
Yet CAD skeptics need to take another look, according to new research conducted by Dr. Matthew Gromet, section chief of breast imaging at Charlotte Radiology, which has a large screening mammography division in Charlotte, NC. To be published in the upcoming April 2008 print issue of the American Journal of Roentgenology, the study compares single reading of screening mammograms without CAD, single reading of screening mammograms with CAD, and double readings.
Gromet's group found that CAD does in fact boost the performance of a single reader, and yields increased sensitivity with only a small increase in the recall rate.
"CAD has changed the landscape of mammography reading," Gromet said. "Double reading is not feasible for most practices, due to cost and manpower constraints. CAD, on the other hand, is widely available and appears to provide comparable benefit to patients."
Dueling studies
In the NEJM study, a multicenter research team led by Dr. Joshua Fenton of the University of California, Davis, found that CAD did not improve the diagnostic accuracy of sites using it (NEJM, April 2007, Vol. 356:14, pp. 1399-1409). Fenton's work found that CAD increased the biopsy rate by 19.7%.
The study sparked a firestorm of debate. It included results from 43 facilities in three states, but CAD was used in only seven of these; it included 429,345 single-read mammograms, but only 7% of these were read using CAD; and different radiologists read mammograms with CAD and mammograms without the technology.
Critics attacked the methodology used in the Fenton study, and expressed concern regarding the time it takes for readers to adjust to using CAD, which was not evaluated in the research.
"It takes an enormous volume of cases to yield enough cancers to prove statistical significance, and it's hard to show any difference between using CAD and not using it if you're dealing with small numbers," Gromet said.
The NEJM findings also contradicted previous research supporting CAD's role in breast screening. For example, in 2001, Dr. Timothy Freer of the Women's Diagnostic and Breast Health Center in Plano, TX, and Dr. Michael Ulissey of the University of Texas Southwestern Medical Center in Dallas screened 12,860 women over the course of a year, using conventional mammography reading techniques as well as CAD. They found almost 20% more cancers with CAD (Radiology, September 2001, Vol. 220:3, pp. 781-786).
The Gromet study
Gromet's research is sure to generate more discussion. Conducted between January 2001 and December 2005, it consists of a review of 231,221 screening mammograms -- a patient population four times that used in the Fenton study. Charlotte Radiology operates 10 sites in the Charlotte, NC, area, and performs 66,000 screening mammograms annually. Until 2003, screening mammograms were double-read; during that year, the group converted to single reading with CAD.
"We practiced double reading for many years, and maintained a meticulous medical audit of our results," Gromet said. "Our audit showed not only that double reading provided a significant benefit in detecting cancer, but also that when we switched from double reading to CAD in 2003, our performance didn't suffer. The transition to single reading with CAD was successful in maintaining high sensitivity -- and we had a lower recall rate than with double reading."
For Gromet's research, screening and diagnostic mammography were strictly separated. All mammograms included in the study were film-screen, taken on Lorad M-IV equipment with Image Checker CL software versions 3.2 and 5.3 (both from Hologic, Bedford, MA).
Out of the total exams interpreted, the same nine radiologists performed the first of two readings in 112,413 patients (48.6%), and a single reading with help from CAD for 118,808 (51.4%). These nine radiologists read a total of 428,909 mammograms during the study period. Annually they read a mean of 9,531 examinations. During the study, their CAD experience included a mean of 13,201. The mean CAD experience of the NEJM study's readers was 821.
"Our study is a historical one, not a prospective, randomized trial -- which would be ethically difficult to implement if randomization included single reading without CAD," Gromet said. "But we made sure that our data came from one program, with the same patient demographics, the same physicians, and the same methodology."
Gromet found that CAD increased sensitivity. Recall rates were comparable between the first reader in the double-read scenario and the single reader with CAD.
The bottom line? Both CAD and double reading are effective ways to increase screening mammography's sensitivity, particularly for experienced readers, according to Gromet.
"Reading a mammogram presents a perceptual challenge," he said. "It's like a 'Where's Waldo?' puzzle, and it's a frequent event not to notice something subtle. CAD's main purpose is to reduce perceptual oversights. The radiologist still has responsibility for the proper interpretation."
By Kate Madden Yee
AuntMinnie.com staff writer
February 13, 2008
Related Reading
Mammo CAD results show reproducibility in serial exams, January 10, 2008
UnitedHealthcare postpones CAD decision, November 27, 2007
CAD vs. radiologist second reads: What's better for screening mammograms? November 16, 2007
UnitedHealthcare ponders cuts to CAD reimbursement, October 26, 2007
CAD still not out of the woods, despite Oregon payor's reversal, July 24, 2007
Copyright © 2008 AuntMinnie.com
|