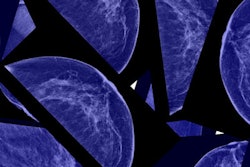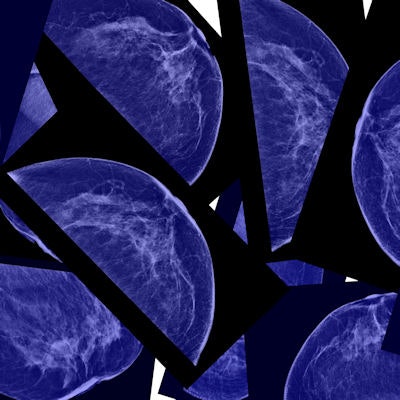
Many small breast cancers will not grow large enough to become significant within a patient's lifetime and, subsequently, finding them early could lead to overdiagnosis, according to a study published in the June 8 issue of the New England Journal of Medicine.
The study questions the value of early breast cancer detection and casts doubt on mammography's efficacy, wrote Dr. Donald Lannin and Dr. Shiyi Wang, PhD, of Yale University. The group based the research on a controversial NEJM study published in 2012 by Bleyer and Welch.
"The recent article by Welch et al in the Journal showed clearly that since the adoption of widespread screening mammography, small breast cancers have increased in incidence over three times more than large cancers have decreased," they wrote. "This implies that many small cancers are not destined to progress to large cancers; instead, their detection results in overdiagnosis" (NEJM, June 8, 2017, Vol. 376:23, pp. 2286-2291).
But there's a problem with the new research, according to Dr. Daniel Kopans of Massachusetts General Hospital: The study's assumptions have no scientific basis.
"This is simply another paper published by a biased NEJM in an effort to reduce access to screening," he told AuntMinnie.com via email. "The paper relies on the estimate of 22% overdiagnosis made by Bleyer and Welch in 2012. It's a complete fabrication, based on fabricated numbers."
Model behavior?
Lannin and Wang analyzed invasive breast cancers diagnosed between 2001 and 2013 in the Surveillance, Epidemiology, and End Results (SEER) database and divided them into three prognostic groups based on biologic factors: grade, estrogen-receptor status, and progesterone-receptor status. The three prognostic groups were defined as favorable, intermediate, and unfavorable, and the biologic factors produced 12 combinations of variables.
The researchers used Welch's proposed overdiagnosis estimate for invasive tumors of 22%. They assumed that the women who fell into the favorable group had the highest rate of overdiagnosis, and those in the unfavorable group had the lowest.
They then generated three virtual populations of women based on age and simulated life expectancies and lead times (defined as the length of time between when a cancer can be detected by screening and when it would have become clinically apparent without screening). For these models, the group also varied distributions of overdiagnosis rates among the prognostic categories:
- Model 1: 41% favorable, 55% intermediate, and 4% unfavorable
- Model 2: 53% favorable, 44% intermediate, and 3% unfavorable
- Model 3: 65% favorable, 33% intermediate, and 2% unfavorable
Finally, Lannin and Wang also varied the overall overdiagnosis percentage, including calculations for 22%, 16.5%, and 11%.
| Estimated lead time and overdiagnosis rates among tumor biologic groups | |||
| Overdiagnosis rate (estimated mean lead time in years) | |||
| Favorable | Intermediate | Unfavorable | |
| Based on a 22% overall overdiagnosis rate | |||
| Model 1 | 40% (19.9) | 22.3% (10.6) | 3.8% (2) |
| Model 2 | 51.8% (29.6) | 17.8% (8.5) | 2.9% (1.4) |
| Model 3 | 63.5% (44.9) | 13.4% 6.4) | 2.1% (0.9) |
| Based on a 16.5% overall overdiagnosis rate | |||
| Model 1 | 30% (13.8) | 16.7% (8.1) | 2.9% (1.4) |
| Model 2 | 38.8% (19) | 13.4% (6.4) | 2.1% (0.9) |
| Model 3 | 47.6% (25.6) | 10% (4.9) | 1.4% (0.3) |
| Based on an 11% overall overdiagnosis rate | |||
| Model 1 | 20% (8.9) | 11.1% (4.4) | 1.9% (0.8) |
| Model 2 | 25.9% (11.6) | 8.9% (4.4) | 1.4% (0.3) |
| Model 3 | 31.7% (14.7) | 6.7% (3.3) | 1% (< 0.1) |
Among women 40 and older, tumors with favorable biologic features made up 38.2% of those that were 1 cm or smaller; tumors with unfavorable biologic features made up 14.1% of those 1 cm or smaller, Lannin and Wang wrote. They noted that tumor size and biologic features both influenced prognosis, with large tumors with favorable biologic features having better prognoses than small tumors with unfavorable features.
The study results "explain both why screening mammography causes considerable overdiagnosis and also why its effectiveness is limited," they wrote.
"Because of the long lead times, mammography is very good at detecting tumors with favorable biologic features, and therefore these tumors are overrepresented among small tumors," they added. "However, many of them do not progress within the patient's lifetime; therefore, they contribute substantially to overdiagnosis. Furthermore, the ones that do progress still have an excellent prognosis even when they become large, so there is little benefit to detecting them early."
Physicians, patients, and the public must be educated on the slow-growing nature of some breast cancers, Lannin said in a statement released by Yale.
"This knowledge will allow us to individualize treatment options, provide 'personalized medicine,' and avoid the major harms of overdiagnosis, which can result in overtreatment and the anxiety and fear that a cancer diagnosis causes," he said.
Scientifically unsupportable?
In response to the paper, Kopans questioned the underlying methodology of the study, in particular its reliance on Bleyer and Welch's assumption that 22% of breast cancers are overdiagnosed -- an estimate that's based on "guesses" and for which there is no actual evidence, Kopans believes.
Studies like the new NEJM one that question the value of mammography screening are having a major negative effect on women's access to breast screening, according to Kopans.
"If these scientifically unsupportable papers continue to be reported as if they simply represent disagreements rather than actually 'alternative facts,' then this [false debate] will continue to go on and women will lose access to screening," he told AuntMinnie.com.