For women who are BRCA1 gene carriers, a combination of MRI and film-screen mammography is the most clinically effective combination for finding breast cancer. But it also costs more, according to a study published in the March issue of Radiology.
Women who are BRCA1 carriers have a higher risk of developing breast cancer. Even though mammography is the current screening standard for the general population, it detects less than half of cancer in high-risk women such as these, according to researchers at Massachusetts General Hospital in Boston.
Dr. Janie Lee and colleagues sought to explore whether the combination of MRI -- which is more sensitive than mammography -- and film-screen mammography (FSM) would be a more effective annual screening protocol for this population. When they compared MRI alone, film-screen alone, and the two modalities used together, the combination of MR and FSM identified breast cancers at smaller sizes and earlier stages (Radiology, March 2010, Vol. 254:3, pp. 793-800). What's more, the combination met defined thresholds for a cost-effective test.
Lee and colleagues used a computer model to compare the three combinations and to estimate quality-adjusted life years (QALYs) and lifetime costs (using 2007 U.S. dollars) in a cohort of 25-year-old BRCA1 mutation carriers. The costs and quality-of-life adjustments were taken from Medicare reimbursement rates and medical literature.
For each strategy, the researchers also calculated an incremental cost-effectiveness ratio (ICER), which describes the cost required to obtain one additional QALY by using the next more effective strategy. In general terms, exams with ICERs less than $50,000 per QALY are considered a good value, while studies that cost more than $100,000 are not considered cost-effective.
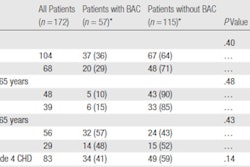
Combined screening was the most effective in terms of quality of life, but also the most costly:
|
In the base-case analysis, ICER to gain an additional QALY through annual combined screening as compared to annual mammography alone was $69,125 per QALY, well within the range of a cost-effective test. Annual MRI imaging was more cost-effective when added as an adjunct to annual mammography rather than used as a replacement.
"Our results support the current American Cancer Society's recommendations to use MRI with mammography [in this population], rather than as a replacement," Lee told AuntMinnie.com.
The trade-off is that adding MRI to FSM for this population boosts the false-positive rate by more than three times: When Lee and colleagues combined annual MR with annual mammography screening in the study models, they found that the number of additional false-positive screening results incurred to avert one breast cancer death rose from 37 to 137.
Women tend to be willing to deal with false positives, however. The group cited a study that found that 63% of women ages 18 to 97 years with no personal history of breast cancer said they would accept 500 or more false-positive screening test results to avoid dying from breast cancer: For women with BRCA1 gene mutations, whose risk is much higher than that of the general population, the benefits of intensive surveillance for breast cancer are likely to outweigh the effects of false-positive screening results projected by the model, they wrote.
"Because combined screening is associated with an increase in false-positive test results, women with increased breast cancer risk should talk with their doctors in deciding whether or not screening with both mammography and MRI is the best individual choice," Lee told AuntMinnie.com.
But the projected cost-effectiveness of annual combined screening depends on the cost of an MR exam and the underlying breast cancer risk of the woman being screened, according to the researchers. When they varied the base numbers used in their model, the advantages of combined MRI and film-screen mammography disappeared.
For example, when the cost of screening MR increased to $960 from the $577 used in the original model, the ICER increased above $100,000 per QALY. Likewise, if the sensitivity of combined screening decreased below 76% (compared to 94% sensitivity in the original model), the combination approach was no longer cost-effective.
"Annual combined screening provides the greatest life expectancy and is likely cost-effective when the value placed on gaining an additional QALY is in the range of $50,000 to $100,000," the authors wrote.
By Kate Madden Yee
AuntMinnie.com staff writer
February 23, 2010
Related Reading
MRI helps find hidden breast cancer, even after US and mammo, January 5, 2010
Rotating breast cancer tests helps high-risk women, December 15, 2008
Getting paid for breast MRI screening -- It's a jungle out there, September 2, 2008
Breast MRI gains momentum for screening high-risk women, September 2, 2008
Combined breast screening provides best survival for BRCA1 mutation carriers, February 26, 2008
Copyright © 2010 AuntMinnie.com