Even among patients at high risk of colorectal polyps and cancer, virtual colonoscopy can be a cost-effective way of finding lesions, according to a study from Denmark. The total costs of virtual colonoscopy (VC) and conventional colonoscopy (CC) were comparable even when the conventional exam and polypectomy were performed on polyps 5-6 mm or larger, according to the researchers. Nevertheless, costs varied significantly based on equipment and the procedures in place at the particular institution doing the exam.
The study, the second in as many months to paint an optimistic economic picture of VC for detecting colorectal polyps, was based on a marginal analysis of 103 patients at two hospitals in Hillerød and Aarhus, Denmark: Copenhagen University Hospital Hillerød and Aarhus University Hospital.
"Even though there is now consensus that CTC (CT colonography or virtual colonoscopy) is useful when CC is incomplete due to an obstructing tumor or for other reasons, the cost-effectiveness of CTC remains to be established," wrote Dr. Regnar Arnesen and his colleagues (Acta Radiologica, April 2007, Vol. 48:3, pp. 259-266).
The study sought to estimate the cost-effectiveness of virtual colonoscopy and subsequent polypectomy, or alternatively conventional colonoscopy alone. The researchers performed a marginal analysis of 103 patients who underwent VC prior to same day colonoscopy at Hillerød (H-I, n = 50) and Aarhus (H-II, n = 53).
The subjects were randomly selected from surveillance (25% at H-I and 32% at H-II) and symptomatic (28% at H-I and 18% at H-II) study populations at the two hospitals, the authors noted. The mean age was 56.98 years at H-1 and 57.8 years at H-II, they added. Six percent of the patients at each institution, 12 patients in all, had been referred for incomplete colonoscopy.
Cost data were obtained prospectively from subsamples of patients in larger randomized and similar observer-blind trials at both hospitals, the authors noted, and effectiveness was based on experience at each hospital.
"Effectiveness was measured as the sensitivities for detection of colorectal polyps ≥ 6 mm (69 in the 148 patients) at H-I, and colorectal polyps ≥ 5 mm at H-II in the same two studies," Arnesen and colleagues noted. "At H-I, the sensitivity was 81% (56/69, 95% CI 70%-90%) for CTC and 87% (60/69, 77%-95%) for CC. At H-II, the sensitivity was 66% (66/100, 57%-75%) for CTC and 93% (93/100, 88%-100%)" for conventional colonoscopy. Patients were excluded for pregnancy, or if they were unable to complete either of the exams or the bowel-cleansing protocol.
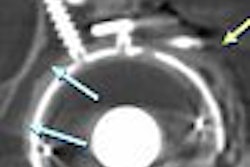
At virtual colonoscopy, performed by a nurse and a radiographer at H-1 and by two radiographers at H-II, all patients were scanned in both the prone and supine positions following colonic insufflation and administration of 20 mg of butylscopolamine bromide (Buscopan, Boehringer Ingelheim, Ingelheim, Germany) and 1 mg of glucagon (Novo Nordisk, Copenhagen). Images were obtained on a four-detector-row scanner (Mx8000, Philips Medical Systems, Andover, MA) at H-II, and with single-slice CT at H-1. The images were examined using a primary 2D approach and a Philips MxView workstation. Same-day colonoscopy was performed with the aid of video colonoscopes.
The cost-effectiveness analysis was based on the cost differential of diagnosing and removing polyps when necessary beginning with VC or conventional colonoscopy, the authors explained. The group compared patient populations, institutions, and procedures at the two institutions.
If a polyp was found at VC but not colonoscopy, the patient was rescoped and any additional polyps added to the ground truth results based on colonoscopy findings.
"Costs were calculated per patient with an identified colorectal polyp (≥ 6 mm at H-1 and ≥ 5 mm at H-II)," they explained. Calculations for VC, colonoscopy, and colonoscopy/polypectomy were made for all 103 patients, and on colonoscopy/polypectomy for the 13 patients with polyps.
"The cost-effectiveness analysis was a marginal analysis including only direct costs that varied between the two alternatives, for example equipment expenses," they wrote. Time spent by healthcare professionals, medicines, and minor equipment were measured prospectively, while salaries and major equipment costs were calculated retrospectively.
According to the results, 13 patients at each hospital had at least one colorectal polyp ≥ 5 mm or ≥ 6 mm, depending on the institution. Virtual colonoscopy was the most cost-effective alternative at H-I (187 euros versus 211 euros), while colonoscopy was the most cost-effective alternative at H-II (239 euros versus 211 euros), the team reported.
"The cost-effectiveness (cost per finding) mainly depended on the sensitivity of CTC and CC, but the depreciation of equipment and the staff's use of time were highly influential as well," the authors wrote.
At both hospitals, significantly more staff time was spent on VC plus colonoscopy/polypectomy compared with VC (p > 0.001), while the difference in time spent on colonoscopy versus colonoscopy/polypectomy was insignificant.
The cost of VC was lower than that of conventional colonoscopy (p < 0.001) at both institutions, and the cost of VC plus colonoscopy/polypectomy when needed was lower than for colonoscopy/polypectomy alone (p = 0 .019 for H-1 and p = 0.115 for H-II).
"At H-1, the cost-effectiveness ratio of CTC was significantly lower than that of CC (126 euros for CTC versus 199 euros for CC, p = 0.001). However, at H-II the difference was diminutive (182 euros versus 183 euros, p = 0.909)," they wrote. "Accordingly, the incremental cost-effectiveness ratio (extra costs per finding) was much higher at H-1 than at H-II, being 1,189 euros versus 187 euros, respectively."
Thus, while the cost of VC was lower than CC at both institutions, the cost of removing detected polyps combined with VC's lower sensitivity rendered the costs equal at only one of the two institutions, the authors explained. And the VC-first strategy may offer the best potential for savings if procedures are also optimized, but "study design, population characteristics, and equipment must be considered as well," the authors reported.
The presence of a nurse to monitor patients before and after colonoscopy contributed to higher costs at H-1, and medication costs were also higher there, possibly explaining the need for more monitoring. Using a single-slice scanner at H-1 may have been partly responsible for shorter interpretation times and lower staff time expenses at that institution as well, the authors suggested. Overall equipment and depreciation costs were similar for both modalities.
Finally, they noted, the polyp cut-off size for CC referral and polypectomy can be expected to significantly affect the cost of VC: the larger the cut-off size, the lower the cost. Technological improvements can also be expected to have major effects on VC's cost-effectiveness.
"Detecting colorectal polyps ≥ 6 mm or ≥ 5 mm with CTC, followed by polypectomy by CC, can be performed cost-effectively at some institutions with the appropriate hardware and organization," Arnesen and colleagues concluded.
By Eric Barnes
AuntMinnie.com staff writer
May 9, 2007
Related Reading
Screening model calls VC most cost-effective colon exam, April 24, 2007
Higher costs seen in post-VC extracolonic follow-up, November 3, 2006
Extracolonic findings double VC costs, but might be worth paying, July 20, 2006
Colorectal cancer screening could add billions to annual healthcare expenditures, November 9, 2005
VC would raise screening costs, study concludes, October 31, 2005
Copyright © 2007 AuntMinnie.com