ATLANTIC CITY - In addition to its diagnostic role, ultrasound can successfully guide therapeutic injections and minimally invasive interventional procedures in sports medicine applications, said Dr. John McShane of McShane Sports Medicine in Villanova, PA.
"Ultrasound has a much bigger future than just being used to diagnose soft-tissue problems," he said. "It really is a guidance tool."
McShane spoke at this week's 2007 Leading Edge in Diagnostic Ultrasound conference.
Several imaging modalities are used in sports medicine. However, most of them have problems, including an inability to correlate patient's feedback with imaging findings, difficulty in comparing the studies side by side, and an inability to image while moving or stressing the injured area, according to McShane. They may also be unable to guide therapeutic interventions such as injections.
On the other hand, ultrasound is easily accessible, relatively quick, and convenient for the patient, McShane said. It also provides excellent resolution of extra-articular soft tissues and allows for dynamic examination.
Multiple studies have demonstrated ultrasound's utility in confirming accurate needle placement for therapeutic injections, such as for a subacromial bursa, the acromioclavicular (AC) joint, and the glenohumeral joint, he said.
Beyond guidance for injections, ultrasound can provide real-time guidance for interventional procedures, according to McShane. This method is well-established in vascular and tumor applications, and can be applied to novel musculoskeletal problems, he said.
Tennis elbow
Tennis elbow, or tendinosis of the common extensor tendon, is a chronic and degenerative condition. Very challenging to manage, it resists most treatment modalities and often has a prolonged course that ultimately leads to surgery, McShane said.
To avoid surgery, many researchers have attempted other, less invasive treatments, such as percutaneous tenotomy. This procedure involves repetitive needling of the abnormal tendon to break up the degenerative scar tissue, he said. Bleeding is created to stimulate healing.
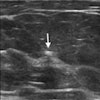
Ultrasound guidance of the procedure can accurately diagnose the problem of tendinosis, identify abnormalities that were not obvious, and precisely guide the needle to ensure that no normal structures are injured and that all abnormal tissue is treated, McShane said.
The lateral epicondyle is usually characterized by smooth bone and a homogenous-appearing tendon. Tennis elbow, however, includes features such as thickening of the tendon, hypoechoic areas, calcifications, bony irregularity, and tears, he said.
With percutaneous needling, the elbow is anesthetized, and the needle is guided through the abnormal region of the tendon. The edge of the bone is abraded, and the tendinotic tissue is repeatedly fenestrated, breaking up the calcification, McShane said.
In a study of 55 lateral elbows with more than six months of pain even after treatment with physical therapy and injections, 80% had good or excellent results following ultrasound-guided percutaneous needling (Journal of Ultrasound in Medicine, October 2006, Vol. 25:10, pp. 1281-1289). McShane and co-author Dr. Levon Nazarian of Thomas Jefferson University (TJU) in Philadelphia are also submitting data on a subsequent group of patients for publication, finding that more than 90% of tennis elbow patients had good or excellent results following the procedure.
"I always said when we started doing this that if I could at least be equal to surgery, if I could be just as good as surgery without all the morbidity and downtime and inconvenience of surgery, then I felt what I had was better," McShane said. "We're actually better than surgery for this problem."
The same basic principle employed with percutaneous needling can be applied to tendons throughout the body, including the elbow, patellar tendon, Achilles tendon, and plantar fascia, he said.
"All of these places develop the same condition, which is tendinosis or chronic degeneration of the tendon," McShane said.
Another area in which ultrasound-guided procedures can perform well is in carpal tunnel syndrome. Surgical treatment for carpal tunnel syndrome involves cutting open the transverse carpal ligament, resulting in decompression of the median nerve. McShane's experience with an ultrasound-guided median nerve decompression procedure, however, has to date resulted in no complications and no recurrences. He is awaiting longer-term outcomes to publish the data.
"This is an example of how ultrasound can be used to guide a procedure that can minimize the invasiveness of the procedure, minimize the morbidity, make it much easier, and have a quicker recovery for the patient," he said.
In the future, ultrasound may replace the arthroscope for certain procedures. "Ultrasound can 'go' places the arthroscope can't go -- soft tissues, for example," McShane said. And instruments will be developed to allow for less invasive treatments, he added.
Ultrasound provides great imaging resolution, helps with guiding injections and procedures, and is easy on the patient, McShane concluded.
"It has a very big future in the realm of sports medicine," he said.
By Erik L. Ridley
AuntMinnie.com staff writer
May 3, 2007
Related Reading
US shows full spectrum of shoulder injuries, September 29, 2006
Focused exams suitable for some musculoskeletal US studies, March 26, 2006
No slam dunk: Partial cuff tears defy MRI, US diagnosis, June 17, 2005
Acromion evaluation proves tricky for x-rays and MRI, February 21, 2005
Copyright © 2007 AuntMinnie.com