When it comes to the frozen shoulder, MRI is good as long as you are happy with static information. But if it's more dynamic information you're after, ultrasound may be a better bet, according to two recent studies. A third paper offered a crash course on making the most of sonography in shoulder disorders, as well as how to identify abnormalities on these exams.
Shoulder impingement syndrome
In the first study, Dr. Nathalie Bureau and colleagues at Université de Montréal in Quebec performed sonography of both shoulders in 13 patients who presented with a clinical diagnosis of subacromial impingement.
Two musculoskeletal radiologists with experience in ultrasound performed the exams, using either a 7.5-MHz transducer or a 5- to 13-MHz one (Sonoline Elegra, Siemens Medical Solutions, Malvern, PA). A standard comparative sonogram was done first so that subacromial impingement could be imaged at 60˚ forward flexion, 60˚ abduction, and 60˚ internal rotation.
For the dynamic exam, "the patient was instructed to elevate the arm halfway between flexion and abduction with the hand in pronation, and the elbow extended was positioned in the coronal plane along the long axis of the supraspinatus tendon, between the acromion and the greater tuberosity of the humerus," the group explained (American Journal of Roentgenology, July 2006, Vol. 187:7, pp. 216-220).
During this active exam, the relationship between the acromion, humeral head, and soft tissues were assessed. If the humeral head passed easily underneath the acromion during shoulder movement, then impingement was ruled out, the authors stated. Otherwise, readers looked for soft-tissue or osseous impingement.
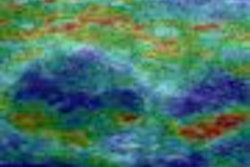
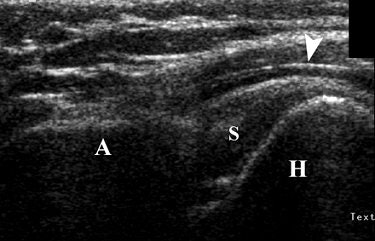 |
| Forty-three-year-old man with upward migration of humeral head during dynamic sonography evaluation of shoulder. Coronal sonography view of left shoulder with shoulder impingement syndrome, during active elevation of arm halfway between flexion and abduction with hand in pronation, shows abnormal upward migration of humeral head (H) in regard to acromion (A), preventing its passage underneath acromion. There is mild distension of subacromial bursa (arrowhead). S = supraspinatus tendon. Bureau NJ, Beauchamp M, Cardinal E, Brassard P, "Dynamic Sonography Evaluation of Shoulder Impingement Syndrome" (AJR 2006; 187:216-220). |
According to the results, there were 14 shoulders with subacromial impingement. In this group, 14% were diagnosed on dynamic sonography and 50% of those were given a grade 3. In the 12 asymptomatic shoulders, 75% were given a grade 0.
"In grade 3 subacromial impingement, there is a failure of the humeral depression resulting in upward migration of the humeral head," Bureau's group stated, adding that possible causes include shoulder joint instability or rotator cuff muscle fatigue.
There were two instances of grade 0 in the symptomatic shoulders, but the authors stressed that these should not be considered false-negative exams as their study did not use a gold standard. Instead, these cases reflected a discrepancy between the clinical diagnosis and the imaging results, serving to emphasize how difficult it can be to diagnose subacromial impingement.
They concluded that dynamic sonography can easily be integrated into routine shoulder imaging protocol as it can provide useful information to the clinician regarding the intrinsic and extrinsic causes of impingement syndrome.
Adhesive capsulitis
Adhesive capsulitis is generally diagnosed clinically, but it can be confused with other causes of shoulder stiffness and pain, according to Dr. Carlos Homsi and co-authors from São Paulo, Brazil.
"This method-validation study showed that (ultrasound) is capable of revealing characteristic morphological changes in shoulders of patients with adhesive capsulitis," wrote Homsi, who is from the Hospital Alemaõ Oswaldo Cruz. Other contributors are from the Hospital Santa Catarina (Skeletal Radiology, September 2006, Vol. 35:9, pp. 673-678).
The patient population consisted of 206 people with ultrasound exams of 498 shoulders. Patients were divided into an asymptomatic shoulder group, a painful shoulders group, and adhesive capsulitis shoulders group based on arthrographic evidence.
Homsi, who has 20 years of experience with musculoskeletal ultrasound, performed all the exams on one of three units with 13-5-MHz linear-array transducers (ATL HDI 5000, Philips Medical Systems, Andover, MA; Sonoline Elegra, Siemens Medical Solutions, Malvern, PA; Logiq 700, GE Healthcare, Chalfont St. Giles, U.K.).
For coracohumeral ligament (CHL) assessment, the patients stood with the shoulder in a neutral position and the forearm extended while being scanned. Scanning started in an axial oblique plane. External and internal shoulder rotation was useful to identify the CHL in the cross-section. A sagittal plane scan was done to obtain a transverse image.
Overall, the CHL was visualized in 66.9% of all 498 shoulders, the authors reported in their results. More specifically, the CHL was seen in 88.2% of the adhesive capsulitis group, in 63% of the painful shoulder cohort, and in 76% of the asymptomatic patients.
In 11.24% of all shoulders, the anatomic variation in the pectoralis minor muscle insertion was seen on ultrasound. In the adhesive capsulitis group, the insertion variation was seen in 11.76% of the cases. In the painful shoulder group, the insertion was seen in 11.94% of the cases. In the asymptomatic group, 9.09% of the patients had this anatomic variation.
A Kruskal-Wallis test for inferential analysis showed that CHL thickness was significantly greater in adhesive capsulitis shoulders (3 mm) than in the other two groups (1.39 mm in painful shoulders, 1.34 mm in asymptomatic shoulders), the authors stated.
"The CHL is shown by US as a linear hypoechoic band, surrounding by hyperechoic fat," they explained. "The overall rate of 66.9% in CHL visualization by US among the three study groups is quite satisfactory." In addition, sonography's ability to identify anatomic variation in the pectoralis minor muscle insertion can prevent it from being misdiagnosed as thickened CHL, they said.
Rotator cuff and beyond
Operator expertise plays a major role in obtaining quality results from shoulder sonography. Advances in technology have improved ultrasound image quality, producing spatial resolution that can exceed that of MRI and without the use of special coils and imaging parameters, explained Dr. Athanasios Papatheodorou and colleagues from the Hellenic Red Cross Hospital in Athens, Greece.
"Also, sonography is inexpensive, fast, and offers dynamic capabilities," they added. "It has been estimated that US is underused for nonrotator cuff disorders.... The strength of US lies in its extreme sensitivity in identification of calcium deposits.... (In this paper) we discuss the various types of rotator cuff and nonrotator cuff disorders that can be sonographically diagnosed" (RadioGraphics, January-February 2006, Vol. 26:1, e23).
The rotator cuff is made up of four muscles and the subscapularis, supraspinatus, infraspinatus, and teres minor tendons. Nonrotator cuff structures encompass several tendons, ligaments, and bursae in the shoulder region.
When performing diagnostic shoulder sonography, the group recommended that a high-frequency (5-12 MHz) linear-array transducer should be used, which gives a spatial resolution of less than 1 mm.
Tendons
Ultrasound images of the tendon should cover the longitudinal and transverse planes. Normal tendons appear hyperechoic relative to adjacent muscles and have an internal fibrillar structure, the group stated. The tendon of the long head of the biceps can be seen within the bicipital groove. The subscapularis tendon should be evaluated in orthogonal planes with the patient's arm in passive external rotation.
For fluid collection assessment in the coracoid process and the various segments of the subscapularis, a lower-frequency probe (3.5 MHz) would work best, the authors stated.
The supraspinatus tendon should be examined with the patient's arm flexed at the elbow and directed posteriorly. The palm should be placed over the posterior iliac crest. The group suggested a posterior approach for visualizing the interwoven infraspinatus and teres minor tendons.
Joints and ligaments
In the glenohumeral joint capsule, the axillary pouch and posterior recess can be seen with a posterior transverse approach using the transducer at a deep setting, the authors stated. An anterior approach should be used to evaluate the coracoclavicular and coracoacromial ligaments. The superior aspect of the acromioclavicular joint capsule appears as a hypoechoic band above the joint on ultrasound.
Rotator cuff disorders
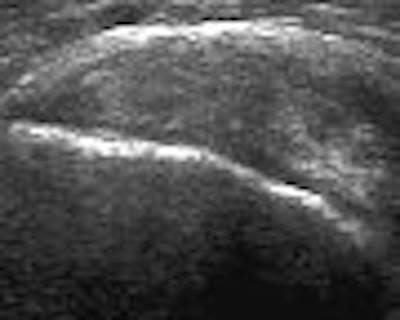
"Most rotator cuff tears occur at the site of insertion of the supraspinatus tendon in the greater tuberosity," Papatheodorou's group wrote. "Essential information for the orthopedic surgeon includes characterization of the tear, the dimensions and location of the tear, and the amount of tendon retraction on the longitudinal view."
Partial tears can occur in the supraspinatus tendon, the bursal side, and the articular side. For full thickness tears, the primary sign on ultrasound is a focal tendon defect or nonvisualization of the focal tendon. Secondary sonographic signs are bone irregularity of the greater tuberosity and the presence of fluid in the joint, they stated. Another sign is cartilage interface or uncovered cartilage.
 |
| Supraspinatus tendon, longitudinal view. The tendon demonstrates a heterogeneous echogenicity without any focal area representative of a tear. This pattern may indicate tendinosis or intrasubstance tear. Papatheodorou A, Ellinas P, Takis F, et al. US of the Shoulder: Rotator Cuff and Non-Rotator Cuff Disorders. RadioGraphics 2006;25:323. 10.1148/rg.e23. Published December 13, 2006. Accessed September 5, 2006. |
Calcium deposits
Ultrasound is very sensitive for detecting very small calcium deposits, the group stated. Calcific tendinitis is caused by calcium hydroxyapatite crystal deposits in various shoulder tendons. On ultrasound, "calcium deposits may have a fluffy appearance, with echogenic foci without posterior shadowing, or may appear as typical discrete, well-circumscribed calcifications with posterior shadowing," they wrote.
Nonrotator cuff disorders
In the long-head biceps tendon (LHBT), biceps tendinosis can be present but ultrasound is only marginally sensitive to this condition. Tendon rupture can occur in either an acute or chronic setting. In the case of the latter, the upper portion of the tendon may not be seen on ultrasound so the authors suggested that the entire length of the bicipital groove be examined.
Joints
In the glenohumeral joint, ultrasound is sensitive to osseous abnormalities that are related to shoulder instability. Sonography is also useful for evaluating the acromioclavicular joint in the superior aspect. The authors suggested that imaging be done in a sagittal plane with a gap between the acromion as a window to visualize the joint space.
Other abnormalities
- Synovial disorders: Multiple small, uniform, echogenic nodules with the joint or bursae, or along the LHBT sheath, on ultrasound.
- Degenerative disorders: On sonography, look for the presence of intra-articular loose bodies and narrowing of joint space in osteoarthritis.
- Chronic hemophilic arthropathy: Ultrasound can assess synovial proliferation, joint effusion, degenerative subchondral erosions, and cysts.
- Benign and malignant tumors: Ultrasound appearance is that of a mass in superficial lipomas and other soft-tissue tumors. For elastofibroma dorsi pseudotumors, sonography shows a mass with a striated appearance and alternating hypoechoic fat strips, surrounded by echogenic fibroelastic tissue.
Finally, Papatheodorou's group pointed out that ultrasound can be used in conjunction with MRI. While the latter offers information on sonographically inaccessible areas, such as bone, labral cartilage, and deep ligaments, ultrasound's strength is its dynamic nature. In addition, sonography can be used in the presence of metal hardware.
By Shalmali Pal
AuntMinnie.com staff writer
September 29, 2006
Related Reading
Focused exams suitable for some musculoskeletal US studies, March 26, 2006
No slam dunk: Partial cuff tears defy MRI, US diagnosis, June 17, 2005
Acromion evaluation proves tricky for x-rays and MRI, February 21, 2005
Copyright © 2006 AuntMinnie.com