VANCOUVER - Radiopharmaceuticals unlocking secrets of the brain, the potential of PET and MRI in breast imaging, and determining the appropriate radiation dose for non-Hodgkin's lymphoma patients are the focus of influential papers at this week's Society of Nuclear Medicine and Molecular Imaging (SNMMI) meeting.
One of the more novel presentations came from Stony Brook University and the U.S. National Institutes of Health, which used PET imaging with carbon-11 raclopride (a molecule that binds to dopamine) to confirm abnormal dopamine response, which, in turn, may lead to obesity.
Abnormal dopamine response to glucose ingestion was found in the brain's nucleus accumbens, considered to be the brain's "pleasure center."
In the study, led by Dr. Gene-Jack Wang, professor of radiology at Stony Brook, 11 healthy controls and eight insulin-resistant subjects consumed a glucose drink on one day and an artificially sweetened drink containing sucralose on another day. After each drink, PET imaging with raclopride was performed.
PET with raclopride showed that subjects who were insulin-resistant and had signs of an eating disorder exhibited remarkably lower natural dopamine in response to glucose ingestion compared to insulin-sensitive control subjects.
"The implications are quite profound," study co-author Dr. Nora Volkow, director of the National Institute on Drug Abuse (NIDA), told AuntMinnie.com. "It shows that it is not the sensation of the taste of the food, but the calories themselves that are driving these responses. It also identified insulin as one of the hormones that evidently modulates this dysfunction of the dopamine signal that drives the behavior."
The findings could help develop interventions, such as medication and lifestyle modification, to help early-stage insulin-resistant people combat obesity and/or diabetes.
"We classically associate the behavior of choosing food because the person decides they want the pleasure or responses of the food," Volkow added. "But our study shows that there is a calorie signal that is improperly signaling the brain's dopamine motivational system that drives the inability to stop. Thus, interventions that aim to ameliorate that are likely to be much more beneficial in sustaining weight reduction."
Tc-99m MIP-1404 imaging agent
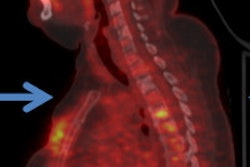
Researchers from Weill Cornell Medical College are showing positive benefits with a novel imaging agent that includes a small molecule of amino acids, called MIP-1404, radiolabeled with technetium-99m (Tc-99m). Used with SPECT, clinicians can see where Tc-99m MIP-1404 binds to a prostate-specific membrane antigen (PSMA) enzyme in metastatic prostate tumors throughout the body.
Led by Shankar Vallabhajosula, PhD, a professor of radiochemistry from the department of radiology, the study revealed that Tc-99m MIP-1404 was well-distributed and ready for imaging as soon as one hour after injection for localization of cancer lesions in bone and lymph nodes. In a majority of cases, Tc-99m MIP-1404 detected more lesions than standard bone imaging.
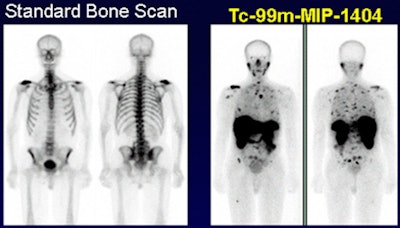 Images show prostate cancer is much more visible with Tc-99m MIP-1404 (right) than with a standard bone scan (left). Images courtesy of SNMMI.
Images show prostate cancer is much more visible with Tc-99m MIP-1404 (right) than with a standard bone scan (left). Images courtesy of SNMMI.Tc-99m MIP-1404 is currently being developed by Molecular Insight Pharmaceuticals, a wholly owned subsidiary of Progenics Pharmaceuticals; the agent is in an international, multicenter phase II trial.
"If a screening can be based on a noninvasive technique, that would be extraordinarily helpful to this patient population," Vallabhajosula said. "Also, once a patient is identified with the cancer and is put on drugs for treatment using this particular imaging biomarker, we can monitor the response to the treatment. That is another interesting opportunity this scan can provide."
Hope for non-Hodgkin's
Accurate estimation of radiation-absorbed dose in radioimmunotherapy based on 3D imaging can lead to extended progression-free survival for non-Hodgkin's lymphoma patients, according to a study from the University of Michigan.
This prospective study, led by Yuni Dewaraja, PhD, an associate professor in the division of nuclear medicine, focused on the correlation between absorbed dose and outcome of radioimmunotherapy with the radiopharmaceutical iodine-131 tositumomab. Researchers conducted dose evaluations on 39 patients with 130 tumors and applied their newly developed model of dose-response analysis.
They found that progression-free survival increased to a median 13.6 months for patients who received a radiation dose of more than 200 cGy. Individuals who received less than 200 cGy had cancer progression after only two months.
By estimating the radiation dose before therapy, information "can be used to customize the treatment to achieve marked improvement in progression-free survival in future studies," Dewaraja said.
However, she cautioned that additional research is needed "to assess the radiation absorption to the bone marrow to make sure there is no high toxicity to this sensitive tissue. We are currently carrying out these studies with SPECT/CT to measure the radiation-absorbed dose in the bone marrow of the lumbar vertebrae area."
Breast PET and MRI
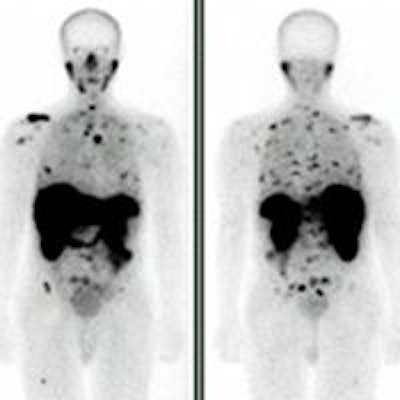
Finally, a study from the Korea Institute of Radiological and Medical Sciences in Seoul has concluded that PET and MRI can improve quality of life and survival for patients with advanced breast cancer by supplying information on the effectiveness of chemotherapy prior to surgery.
All subjects underwent three cycles of neoadjuvant chemotherapy and sequential whole-body FDG-PET/CT, breast MRI, and delayed breast PET/CT four times. Scans were performed prior to the first course of chemotherapy, after the first round, after the second course, and one more time prior to surgery.
Patient survival with no recurrence of cancer after neoadjuvant chemotherapy ranged from slightly less than three months to approximately three years, resulting in a median of 661 days with no recurrence.
Lead researcher Dr. Sang Moo Lim, director of the department of nuclear medicine, and colleagues said the modalities may be applied to other malignancies and could lead to improved clinical outcomes.
"Considering the results of our research, we now need to further develop the technology -- not just imaging systems, but tracers and biomarkers -- to advance our field," Lim said.