LONDON - PET/CT prior to radiotherapy can help oncologists target a more powerful dose of radiation to non-small cell lung cancer (NSCLC), whilst keeping dose low in other areas of the organ, according to research presented at this week's European Society for Therapeutic Radiology and Oncology (ESTRO) meeting.
Dutch researchers wanted to address the thorny problem of "radioresistant" tumors, or cancers that don't respond to radiation therapy delivered at conventional levels. But the concept isn't truly an accurate one, as all tumors will respond to radiation assuming the dose is high enough, according to Dr. Dirk De Ruysscher from the Maastro Clinic at University Medical Centre Maastricht.
"Radioresistance doesn't really exist in the pure sense; it's a matter of dose and timing," he said. "Stage III NSCLC is heterogeneous, with poor survival and poor local control, but even in these tumors, improving local control can improve survival."
The trick is finding a way to increase dose without affecting the organ at risk. That's where FDG-PET/CT can help by identifying areas within the tumor that might be resistant to treatment.
"By using PET, it's possible to increase radiation dose by decreasing radiation field without increased side effects," De Ruysscher said. "It is quite remarkable that this holds true for stage III NSCLC as it does for all stages."
When De Ruysscher and colleagues tested the theory in a phase II study, they irradiated lymph nodes that were positive for cancer on PET scans and monitored local recurrence. "We found only 2% isolated node failures when based on PET-positive lymph nodes," he said.
Following this, an individualized dose escalation study combined selective nodal irradiation based on FDG-PET scans with short overall treatment time based on a certain mean lung dose (MLD) up to around 90 Gy. Results, published in the Journal of Clinical Oncology, showed approximately 45% survival, and a further publication will show 55% survival with concurrent chemoradiation at two years.
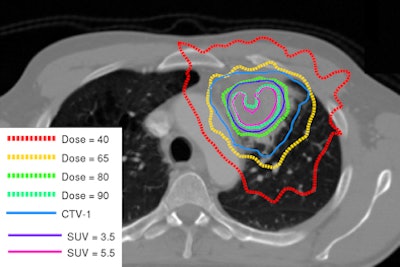
Next, the group decided to investigate dose escalation when delivered "inhomogeneously." NSCLC tumors are heterogeneous in composition, so delivering equal doses across a tumor provides too low a dose to resistant parts, and overkill to more sensitive parts.
"It's more logical to give a heterogeneous dose distribution to a heterogeneous tumor for optimized local control," De Ruysscher said.
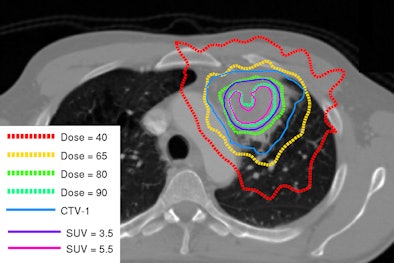 |
| Image shows redistribution of dose according to tumor heterogeneity. Courtesy of Dr. Dirk De Ruysscher. |
An ongoing phase II randomized trial investigating dose redistribution is being conducted with the Netherlands Cancer Institute. Instead of a flat radiation dose across the tumor (all greater than 4 cm for local tumor control), dose is increased in the FDG-positive areas. A radiation dose of 90 Gy in 24 fractions was given to some areas without subjecting normal tissues to an increased dose.
"In the inhomogeneous dose group, nodal areas received 66 Gy in 24 fractions, whilst FDG-positive areas received the highest dose possible, similar to stereotactic body radiation therapy," he said.
De Ruysscher will also investigate the value of hypoxia-related PET scans and delayed contrast-enhanced CT scans looking at blood flow, permeability, and blood volume, and correlate these metrics with FDG and hypoxia signals to understand what is happening in patients on both very high and homogeneous doses.
"We've found that hypoxic areas overlap with FDG-positive areas by up to 80%," he said.
After the presentation, an audience member questioned whether it was necessary to acquire hypoxia measurements with CT given the availability of FDG uptake information.
"A metabolic response is much better than a CT response, and that shows an important prognostic value, but I think that we need data before or early in treatment and then dose-escalate in some cases," De Ruysscher said. "We chose to image pretreatment because we believe short imaging time is important, and adaptation after three or four weeks means overall treatment time is longer."