When the clinical indications for ordering a CT chest exam receive a high "appropriateness" score from a clinical decision-support system, the probability that the exam will be positive is also high, according to a study presented at the American Roentgen Ray Society (ARRS) meeting in Vancouver.
Massachusetts General Hospital (MGH) in Boston pioneered the use of clinical decision-support systems, integrated with computerized physician order-entry (CPOE) software, for radiology procedures. As part of continuing research, imaging informatics research fellow Dr. Supriya Gupta reported findings on the validity of chest CT exams ordered using the clinical decision-support system.
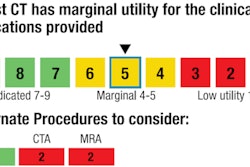
The software at MGH requires that physicians provide information about clinical indications, relevant prior medical history, and reasons for ordering the exam. After this information is entered, the software produces a "utility score" for the ordering physician (high, medium, or low), and when applicable, it provides alternative exams that may be more appropriate. Physicians may overrule the advice of the software, but many heed it.
In Gupta's study, researchers assessed the degree of correlation between the appropriateness score and findings in CT chest exams performed between 2005 and 2010. Of the 93,818 chest CT exams ordered using the decision-support system, 76% of the patients had a positive finding.
Commonly selected indications for ordering chest CT were the identification of a nodule on a previous exam (18%), primary lung cancer (12.6%), and known metastasis (13%). Additional indications included an abnormal chest radiograph (7.5%), persistent cough (7%), shortness of breath (5.1%), lymphoma (4%), and complaints of fatigue (3%).
Appropriateness scores were highest when abnormal chest radiography or shortness of breath was indicated, Gupta said. Persistent cough, fatigue, primary lung cancer, or a previously identified nodule also produced high-ranking scores.
"We confirmed that when common indications are selected for performing a chest CT exam, the appropriateness utility score also tends to be high, and radiology report findings show that performing the exam justified both the radiation dose exposure to the patient and the cost of the exam," she said.
Among the nearly 100,000 exams, 87% of those with high utility scores had positive report findings. Only 12% of the exams with low utility scores had positive findings.
Fewer than 1% of the exams received an intermediate score. "We think this is because ordering physicians are presented with other types of exams that evidence-based guidelines indicate are more appropriate," Gupta said. "Based on findings of this study and others we've conducted, we think that they select the other options."
As part of the study, Gupta and colleagues analyzed the reports of exams that had a low utility score but a positive finding. The vast majority of the 12% represented rare clinical indications that weren't included in the clinical decision-support software.
"A patient with a glioblastoma is one example that comes to mind," she told AuntMinnie.com.
Gupta also said that such outliers are routinely reviewed, and feedback is provided to referring physicians who may be ordering diagnostic exams that prove to be of no value for their patients.
"Rising concerns about radiation risks, imaging growth, and reimbursement costs have highlighted the need to curtail inappropriate imaging use," she said. "We think that at some point the need to integrate clinical decision-support systems with CPOE will become an integral part of meaningful use requirements."