When a medium-sized imaging center decided to achieve a paperless clinical work environment when replacing its aging RIS, it expanded this goal to include patient interaction as well. One year later, this decision has paid off handsomely.
The patients of Valley Regional Imaging in Fayetteville, NC, won't find ballpoint pens and paper forms at this facility. Instead, they'll be greeted with a friendly smile and invited to an interactive pen display cubicle. This electronic technology expedites registration workflow, reduces a variety of operational expenses, and has almost completely eliminated clerical errors, omissions, and accidental retention of incorrect patient information, according to the outpatient imaging center.
Valley Regional Imaging is a full-service center, offering CT, MRI, ultrasound, radiography, fluoroscopy, mammography, and bone densitometry examinations, averaging 3,300 patient visits a month. Exams are read by 21 subspecialty radiologists.
When the center was established in May 2009 as a joint venture of Cape Fear Valley Health System and Carolina Regional Radiology, it acquired an existing outpatient imaging facility which included a leased RIS and PACS. The staff quickly discovered that the RIS was underautomated and labor intensive, with many manual processes built into it. It was time for a change, according to executive director Rhonda Mayorga, PhD.
 Patient at interactive pen display cubicle. Image courtesy of Valley Regional Imaging.
Patient at interactive pen display cubicle. Image courtesy of Valley Regional Imaging.A new RIS (MedInformatix) and PACS (Intelerad Medical Systems) became fully operational in July 2010. Just a few months earlier, Mayorga investigated whether interactive pen displays could eliminate the need for patients to complete paper forms and consent documents.
She and her colleagues liked what they saw, but they couldn't kick the tires and try out the product due to issues with the existing RIS. They went ahead and purchased five displays (Wacom Technology), taking a gamble that patients and the registration/clinical staff would like it, and that it would work as promised.
"We knew that we could expedite the registration process significantly, and we were convinced that our patients would appreciate having less paperwork to deal with at each visit," Mayorga said. "Each patient's registration involved completing multiple patient forms. Patients also had to complete medical record-related forms for examinations that a patient had to finalize with the radiologic technologist. These would include a combination of screening questionnaires, history forms, contrast forms, and consent forms. Because all these documents had to be scanned into the RIS, we thought that our staff would be pleased as well to have this work eliminated."
All this proved to be true. The interactive pen displays interfaced into the RIS as promised and worked as promised.
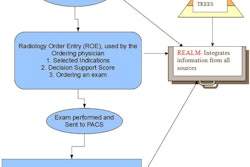
When a patient arrives for an exam, the center's receptionist checks the patient in at the RIS. The RIS displays a "registration tree" that lists all associated documents and forms that the registration clerk can select based on the appropriate exam. Between 30 and 40 forms were incorporated into the new RIS for use in the clerical and clinical areas. Examples include a patient demographics form, patient consent forms, work release forms, insurance forms, Medicaid verification, HIPAA privacy forms, authorization for release of images, medical records release/receipt forms, and many more.
Once checked in, the patient is invited to a cubicle and either enters demographic data for a new patient or confirms that the existing RIS information that populates the form is correct. Patients can make modifications themselves or ask the clerk to do it for them, and they sign the form using the electronic signature box and an interactive pen. All other forms needed for the exam are competed in the same manner.
On average, the process takes five minutes; previously, it averaged 15 to 20.
"All of our patients, regardless of age, have quickly adapted to the new technology," Mayorga said. "They are able to clearly see and read the large screen display, and they find the pressure-sensitive pen easy to use when signing documents. None have complained or felt insecure about completing and signing documents electronically."
In addition to being able to process patients much more rapidly, technologists who had forms to complete that in some cases needed to be signed by patients also found that the process was expedited by the tablet PCs and electronic pens.
The center tracked cost savings. From January 2010 to July 2010, when the former RIS was being used, the administrative cost to process 19,694 patients was $66,960. From August 2010 to May 2011, 31,504 patients were processed at a cost of $26,778. The cost of processing a patient dropped from $3.40 per patient to 85 cents.
The salary cost to scan documents in 2010 was $5,160, representing 430 hours of labor. This expense has been eliminated, Mayorga said.
In spite of best efforts, paper has not been completely eliminated. It is necessary, for example, to still mail letters to mammography patients. However, this cost has been reduced by 55%, averaging $95 per month in 2011, compared with $195 in 2010. This represents an annual savings of $1,200, according to Mayorga.
Similarly, shredding costs have been reduced by 73%. The center has only one outside shredding service pick-up per month, and it projects an annual savings of approximately $1,300.
"While many costs seem small, they all add up and contribute to the return on investment for purchasing the RIS," Mayorga concluded. "Our business has been streamlined, and as an added plus, our operations are greener with respect to environmental impact."