Serious discrepancies in image interpretation are fairly rare among residents in trauma centers, particularly in the third and fourth years of training, concludes a multiyear study conducted at a tertiary care center in Virginia. Results were published online in Emergency Radiology.
The exhaustive review found a miss rate ranging from 0.23% to 0.42%, which is toward the lower end of discrepancies reported in previous research, wrote researchers from Eastern Virginia Medical School in Norfolk. In general, the group found far fewer misses after the first two years of residency. Among typically missed findings, fractures on both radiography and CT topped the list, followed by hemorrhages on CT and pulmonary nodules and infiltrates at x-ray.
"Our residents do have a low overall discrepancy rate, which is nice, and it was in line with what had previously been found in other programs," said lead author Dr. Jennifer Tomich in an interview with AuntMinnie.com.
Most frequent discrepancies
The researchers sought to identify the most frequently reported on-call discrepancies at the hospital by modality and level of resident training, wrote Tomich and co-authors Dr. Michele Retrouvey and Dr. Sarah Shaves.
"Our intent is to identify specific areas of concern that may be amenable to improvement through initiation of dedicated resident training in the field of emergency radiology," they wrote (Emergency Radiology, July 26, 2013).
"We had multiple things we were trying to look for; a lot of studies that came before it were a little bit limited, and they were only very specific misses that radiology residents had made," Tomich said. "A lot of studies had limited themselves to one modality or something very specific. We wanted to identify for all radiology residents if there were specific things that everybody seemed to have difficulty with, versus the new call takers."
Residents provide "wet reads" on emergency imaging studies obtained during evening, overnight, weekend, and holiday hours at academic teaching centers across the U.S. These are reviewed by an attending physician who notes significant misses or discrepancies for internal quality control.
Residents at the authors' 525-bed facility take call from 5 p.m. to 7 a.m., as well as on weekends and holidays. The residents cover all modalities, though the on-call attending performs urgent MRI reads and inpatient diagnostic studies.
The current study examined a large dataset collected over seven years. The sample of 193,722 dictated studies included 103,292 x-ray exams (53.3%), 81,537 CT exams (42.1%), 7,787 ultrasound studies (4%), 484 nuclear medicine studies (0.3%), and 446 fluoroscopy studies (0.2%). In 0.1% of studies the modality was not specified, and five of the 653 discrepancies were eliminated because the type of study couldn't be identified, the authors wrote.
The reported discrepancy rates (0.23% to 0.42%) were low for all levels of training, but they were especially low for senior residents in years three and four. The highest discrepancy rates were seen in R2 and R1, with no statistically significant difference between the two years, Tomich and colleagues wrote.
This was followed by a small but statistically significant drop in the miss rate between R1/R2 and R3/R4 levels (p < 0.05); there was no statistically significant difference between R3 and R4. The way call responsibilities transitioned probably affected the improvement rates, Tomich said.
"It used to be that people started taking call halfway through their first year of residency, but [the Accreditation Council for Graduate Medical Education (ACGME)] changed the rules so that first years are no longer allowed to take call," she said. "Our study covers both sides of the transition and thus may have slightly distorted the data, so it looks as though there were periods of little progress when that was not necessarily the case."
As for fourth-year residents performing similarly to third years, many fourth-year residents took less call that year because they were studying for the boards, Tomich said; as a result, they may have experienced periods in which they were a little less confident. The study did not analyze whether gaps in call led to an increase in discrepancy rates, however.
By modality, discrepancy rates were highest for nuclear medicine studies at 0.62%, followed by CT at 0.49%, x-ray at 0.25%, fluoroscopy at 0.22%, and ultrasound at 0.12%. Of the fractures missed on radiographs, phalangeal fractures of the hand were the most common, at 15, followed by metatarsal fractures in the feet, with 10 misses.
"Metatarsal fractures and lung nodules on x-ray were commonly missed at all levels of training. Some reads are just hard," Tomich said.
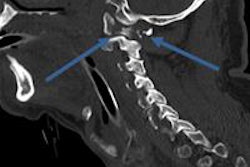
On CT, the most commonly missed fractures were of the rib (n = 12), and intracranial hemorrhage was the most common vascular miss, led by subdural hemorrhage (n = 9) and subarachnoid hemorrhage (n = 8).
"It is interesting ... that the intracranial hemorrhage category demonstrated similar levels of reporting for the R1 through R3 levels, indicating that difficulty with this category was not isolated to new call takers," the study team wrote. Lung nodules (5%) and pulmonary infiltrates (4.8%) on radiographs were the most common chest discrepancies.
| Overall missed findings by category and modality | |
| Modality | Percent missed |
| Fractures on radiographs | 15.2% |
| Fractures on CT | 14.1% |
| Masses on CT | 6.2% |
| Hemorrhage on CT | 5.3% |
| Lung nodules on x-ray | 5.0% |
| Pulmonary infiltrate on x-ray | 4.8% |
| Lacerations on CT | 2.3% |
| Brain infarction on CT | 2.0% |
| Bowel wall thickening on CT | 1.9% |
| Pulmonary embolism on CT | 1.9% |
| Other/miscellaneous | 38.4% |
Overall, the most common categories of discrepancies appear to be similar, with fractures and lung nodules/infiltrates accounting for a significant proportion of the misses reported for every level of training, the authors wrote.
One limitation of the study is the subjective nature of what constitutes a significant miss, they noted. The other significant potential limitation is the risk of underreported discrepancies. "If the attending missed it as well as the resident, then it wasn't covered in our study," Tomich explained. The fact that residents had an on-call radiology attending and an ultrasound technologist available for consultation also could have lowered the number of reported discrepancies, according to the authors.
The study showed an overall discrepancy rate of 0.3%, compared with the generally higher previously reported rates of 0.2% to 2.6% in smaller studies. The similar rates of discrepancies for residents in their first two years likely reflect that there are new call takers in both of those years of training.
Radiology resident training programs should ensure that common discrepancies are specifically addressed as part of a dedicated emergency radiology course, the authors concluded.