When federal authorities released draft guidelines for stage 2 of the U.S. government's meaningful use stimulus program earlier this year, they were widely seen as favoring primary care physicians over medical specialists. Last week, specialists -- including radiologists -- got the chance to make their case for better representation.
In a May 13 meeting in Washington, DC, before the Meaningful Use Workgroup of the Office of the National Coordinator for Health Information Technology (ONC), representatives from five medical specialties offered their final pitch for changes to the draft stage 2 guidelines before final versions are submitted in June.
In attendance were representatives from radiology, pathology, ophthalmology, surgery, and allergy/asthma/immunology specialties. Of the groups, representatives from radiology and pathology made similar arguments:
- Radiologists and pathologists pioneered the adoption of electronic recordkeeping decades ago, and the overwhelming majority of these specialists "meaningfully use" these technologies on a daily basis.
- Technology that already exists and works successfully should be incorporated into the stage 2 meaningful use criteria recommendations.
- Medical specialists should not be required to purchase electronic capabilities they do not need and will not use to qualify for incentive payments from the federal government.
The Friday hearing followed a meeting hosted by the U.S. Department of Health and Human Services (HHS) Health IT Policy Committee earlier in the week, at which the Meaningful Use Workgroup presented a revised draft proposal for stage 2 criteria. Whether the facts and recommendations made at the May 13 meeting will sway the workgroup to make additional modifications to the final proposal it will submit on June 8 to the HIT Policy Committee is unknown.
But Dr. Keith Dreyer, PhD, co-chair of the American College of Radiology's (ACR) IT and Informatics Committee, and Dr. David Booker, governor of the College of American Pathologists (CAP), both made strong arguments that additional changes are needed.
The objective of the meeting was to hear testimony that would help the Meaningful Use Workgroup formulate recommendations to the HIT Policy Committee and the National Coordinator on the needs of specialty practices. In addition, the goal was to learn about the experiences of healthcare practitioners and hospitals currently operating in an electronic world, stated workgroup chair Dr. Paul Tang, vice president and chief innovation officer at the Palo Alto Medical Foundation. He said that the information would inform the workgroup's deliberations on stage 2 and stage 3 meaningful use objectives.
"The invitation was significant because it's the first time a radiologist was formally invited by ONC to participate in a public federal advisory committee hearing on meaningful use. Most other major specialties were not invited to be at the table, unfortunately," Michael Peters, ACR assistant director, regulatory and legislative portfolio, told AuntMinnie.com.
The workgroup wanted to learn how specialists leverage electronic health records (EHRs) to fully participate in the continuum of patient care. It wanted to hear about the experiences of both primary care providers and specialists in implementing electronic records, and how that can contribute to stage 2 criteria. It also wanted to learn how EHRs facilitate how specialists manage patient populations, including performance measurement and feedback. Finally, it was interested in how EHRs facilitate specialty care of individual patients, including the use of clinical decision-support systems.
ACR comments
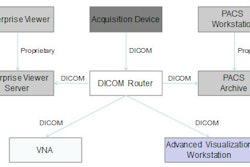
Dreyer noted that an estimated 85% of all U.S.-based radiologists already used RIS and PACS on a daily basis, and that many healthcare facilities use simple Web protocols to insert images into their EHRs for use by affiliated physicians and clinical staff. "Through its rapid adoption over the past decade, the value of this digital medical imaging technology and its integration to the EHR has become essential to the clinical care of patients," he said.
"The challenge today is incentivizing those same facilities to share their image data with other neighboring medical facilities as well as the patients themselves," he told the workgroup. CDs are used to transfer images from one facility to another, but "a preferred and fully realizable approach, if incentivized through a mechanism like meaningful use, would be true electronic exchange."
Quoting Dr. David Blumenthal, former ONC national coordinator for healthcare IT, who stated in January 2011 that "we can't have an effective EHR system that can't move images," Dreyer reminded the committee of a 2011 meeting that ONC co-sponsored with the National Institutes of Health (NIH) that explored capabilities and opportunities related to diagnostic imaging.
"The resounding take-home messages from that ONC-NIH meeting were that the capabilities and standards exist now, image and imaging data exchange is a critical component of EHR technology, and that imaging-related information should be implicitly included in meaningful use criteria because of its importance to the diagnosis and treatment of patients," he said.
Dreyer also described both the patient safety and financial benefits of using clinical decision-support systems interfaced with computerized physician order-entry (CPOE) systems. He also emphasized the contradiction that stage 1 CPOE certification criteria require systems to have the functionality to order radiology exams; however, this is not a requirement of stage 1 meaningful use requirements. Requiring CPOE without use of clinical decision-support tools will not be as effective either.
Adding these requirements to stage 2 is a no-brainer because "the solutions already exist and are in clinical use," according to Dreyer. "These tools have years of supporting evidence behind them and are ready for prime time in stage 2 meaningful use."
Dreyer concluded by stating the ACR's position that healthcare coordination, efficiency, and quality improvement would be best achieved through meaningful use requirements that are relevant to medical specialties.
"Specifically, the Centers for Medicare and Medicaid Services [CMS] and ONC should provide meaningful use functionality objectives and measures that will improve medical imaging care, including functionality measures for structured reporting, communication of critical findings, access to key image data, and recording and monitoring of radiation dose," he said. "These types of specialty-centric functionality measures should be used in place of other meaningful use measures that have no bearing on radiology practices today and will distract radiologist eligible providers from implementing technology that will improve specialty care of patients."
Pathology comments
Representing clinical pathology, Booker reiterated the same message. Stating that pathology was also one of the first specialties to embrace healthcare IT, he pointed out that sophisticated computerized laboratory information systems (LIS) are ubiquitous in healthcare facilities and freestanding medical laboratories throughout the U.S.
"If the idea behind meaningful use is to incent adoption of the appropriate electronic clinical system, such an incentive is unneeded in pathology given essentially universal adoption of LIS and related health IT systems in pathology practice and laboratories," Booker said.
Pathologists don't directly use EHRs to input data, according to Booker. "The meaningful use rules as currently written are fundamentally not applicable to pathology," he said. He also pointed out that according to the CMS final stage 1 rule, pathologists qualify as eligible providers. This means that while they cannot qualify for meaningful use incentives, they do qualify to be penalized for not adopting them. Booker asked the workgroup to recommend that pathologists be exempt from the meaningful use penalties that commence in 2015.
What about other medical specialties? Few were invited to state their case. But from Michael Peters' perspective, "all nonprimary care specialists are in the same boat in terms of finding meaning in meaningful use. The concern about clinical relevance continues to be more or less universal."
Details of the hearing can be accessed here.