Fifty-two of the largest and most influential medical professional societies and organizations in the U.S. have united to recommend major changes in the electronic health record (EHR) incentive programs proposed by the Obama administration.
In a letter dated May 3, 2010, to Kathleen Sebelius, secretary of the U.S. Department of Health and Human Services, the societies identified omissions, inconsistencies, and barriers in the Centers for Medicare and Medicaid Services (CMS) proposed rule on the Medicare and Medicaid EHR incentive programs. The letter's objective was to ensure that the provisions of the American Recovery and Reinvestment Act (ARRA) of 2009 are implemented in a manner that will promote the widespread adoption of health information technology.
Organizations representing diagnostic imaging and radiation therapy interests included the American College of Radiology, American College of Radiation Oncology, American Society for Radiation Oncology, and SNM.
More time to 'meaningful use'
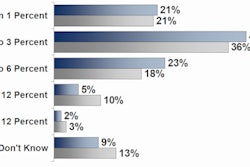
The societies requested that CMS allow providers to implement a percentage rather than all of the currently stated requirements for demonstrating "meaningful use," a provision in the ARRA that requires funding recipients to prove that their healthcare IT projects produce real clinical benefits. The societies also want providers to have greater flexibility in choosing which requirements to implement, and they've requested that the time period to achieve meaningful use criteria be extended to 2017 to be consistent with the ARRA.
Pointing out that the proposed CMS rule takes an inflexible "all-or-nothing" approach, where failure to meet any one of the two dozen requirements means the provider would not receive funding, the societies stated that very few providers would be able to meet this requirement even if they had succeeded in adopting many of the required EHR components.
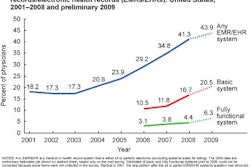
The proposed meaningful use requirements were also criticized for being unrealistic and failing to acknowledge that providers adopt EHR functions incrementally and in differing order. The societies noted that advanced functions, such as computerized physician order entry (CPOE), clinical decision support, and electronic medical reconciliation, all generally are implemented at the end of a multiyear transition to EHRs.
Change definition of a hospital
ARRA currently defines a hospital as a Medicare subsection (d) hospital, which is a general, acute-care, short-term hospital. CMS proposes to provide incentive payments to hospitals as identified by their Medicare provider number.
The societies requested that for the purpose of ARRA healthcare IT incentives, CMS should define a hospital as a discrete facility of service. This would eliminate the problem facing hospital enterprises with a single Medicare provider number, whose individual hospitals might be utilizing different IT systems and be at different stages of EHR implementation. Combining meaningful use requirements for multiple hospitals that have autonomous EHRs, because they are part of a larger healthcare enterprise, could jeopardize financial incentive payments if a sole hospital failed to achieve EHR adoption goals in a timely fashion.
Long-term-care facilities may be discriminated against when they would, in fact, benefit from EHR adoption. The societies also requested that critical access hospitals, of which 1,300 serve patients in rural areas of the country, be able to qualify for Medicaid EHR incentives.
Small physician practices
The societies pointed out that small physician practices represent 80% of all outpatient visits, yet none are members of the Health Policy IT Advisory Committee. The societies requested representation for this group of healthcare providers.
They also requested that physicians receive feedback on their EMR implementation performance, so they know if they are meeting the criteria for incentive payments.
The societies recommended that CMS only require reporting of healthcare IT functionality measures that can be generated directly from EHRs. Many of the proposed healthcare IT functionality measures, including orders placed using CPOEs, electronic prescriptions, and laboratory reports entered as structured data, would require 100% manual review, according to the societies. Additionally, software for many quality reporting measures proposed by CMS has not yet been developed by vendors.
The societies stated that the current proposed requirement of maintaining evidence of qualification to receive incentive payments for 10 years after registering for the incentive program was "unacceptable." Citing cost and potential storage media technology obsolescence, they requested that the retention period be halved.
The letter sent to the Department of Health and Human Services may be read by clicking here.
By Cynthia E. Keen
AuntMinnie.com staff writer
May 10, 2010
Related Reading
Radiology societies comment on HIT stimulus, March 17, 2010
Don't ignore imaging when planning healthcare IT stimulus goals, March 9, 2010
Hospitals need to scramble on stimulus fund goals, March 3, 2010
HIMSS vendors chase 'meaningful use' -- and stimulus dollars, March 2, 2010
Copyright © 2010 AuntMinnie.com