Multimedia radiology reports that provide hyperlinks to annotated tumor measurements and include graphs that show treatment response can improve how these lesions are tracked over time, according to research published as a web-exclusive article in the February issue of the American Journal of Roentgenology.
In a retrospective study involving nearly 500 lesions, a team from the U.S. National Institutes of Health (NIH) Clinical Center found that multimedia reports significantly improved concordance between radiologists and oncologists in selecting and measuring target lesions, compared with text-only radiology reports. The result is fewer discrepancies between what radiologists are measuring and what the oncologists are using to evaluate how these tumors are responding to therapy.
"Thus, multimedia-enhanced radiology reports provide more information for oncologists than text-only radiology reports," wrote the NIH team, which included first author and postdoctoral research fellow Dr. Laura Machado and senior author Dr. Les Folio (AJR, February 2017, Vol. 208:2, pp. W31-W37).
Selecting, measuring lesions
While cross-sectional imaging and objective criteria such as the Response Evaluation Criteria in Solid Tumors (RECIST) are used to assess tumor burden in cancer patients in oncology clinical trials, radiology reports don't often include the necessary measurements of target lesions. Even if these measurements are available, they frequently don't match those in the oncology records that are used to calculate therapeutic response, according to the authors.
In recent years, the NIH group collaborated with PACS vendor Carestream Health on a PACS upgrade that offers the ability to embed hyperlinks, tables, and graphs into the radiology report. With these multimedia reports, clicking on the hyperlinked measurement in the report opens up the annotated measurement in that particular CT slice and series.
The researchers published a study in the October 2015 issue of AJR that found both radiologists and oncologists preferred having those links in the reports. What's more, a study presented at the RSNA 2015 meeting found that the multimedia report led to an average of nearly nine minutes in time savings for the oncologist to assess tumor burden.
In a paper published online January 10 in the Journal of Digital Imaging, the NIH team also shared its Exportable Notation and Bookmark List Engine (ENABLE), an interface the researchers developed to export measurement metadata from PACS to prepopulated digital RECIST worksheets for the electronic medical record (EMR) and cancer databases, Folio said.
"[Offering] improved consistency of target lesion selection and measurements, our multimedia-enhanced radiology reports are more informative, with crucial information readily available by linking from the report to the images," Folio told AuntMinnie.com. "At the same time, [the] measurements radiologists and radiology assistants make in PACS can now be exported directly after the oncologist's verification, obviating the need for handwriting on RECIST forms or remeasuring on third-party software platforms."
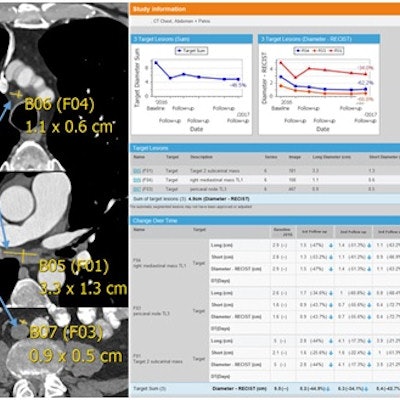
Under the new workflow, target lesion measurements on follow-up chest CT exams are compared with measurements on the baseline CT exam. A radiologist assistant is empowered to close communication gaps between oncologists and radiologists by verifying target lesion selection and ensuring that the proper baseline data are set in the PACS software, according to the group. The resulting multimedia radiology report includes measurements of targeted lesions along with automated RECIST 1.1 calculations, presented in tables and graphs that show changes in lesion size over time.
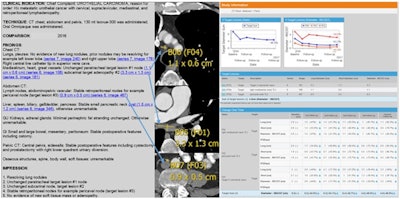 Example of a multimedia radiology report for three metastatic (urothelial cancer) target lesions that have been followed over a year and show partial treatment response in accordance with RECIST 1.1 criteria. The graphs depict tumor shrinkage over time; the left graph includes all three tumors, while the right graph shows three individual target lesions. Image courtesy of Dr. Les Folio.
Example of a multimedia radiology report for three metastatic (urothelial cancer) target lesions that have been followed over a year and show partial treatment response in accordance with RECIST 1.1 criteria. The graphs depict tumor shrinkage over time; the left graph includes all three tumors, while the right graph shows three individual target lesions. Image courtesy of Dr. Les Folio.Clinical value?
In the current study, the researchers sought to assess the clinical value of hyperlinked tumor measurements in these multimedia reports. They also wanted to evaluate the merit of including a radiology assistant in this process of assessing tumor burden.
They retrospectively assessed CT exams of the chest, abdomen, and pelvis in 71 consecutive metastatic genitourinary cancer patients who were enrolled in two therapeutic clinical trials from September 2015 to February 2016. The patients had 489 target lesions on 232 CT studies.
A radiologist assistant -- a postdoctoral research assistant -- compared the target lesions selected by the oncologist with the lesions reported in the final text-only or multimedia radiology reports. Next, the radiologist assistant determined how many of the target lesion measurements in the reports matched the target lesion measurements recorded in the oncology records that are used to calculate therapeutic response.
| Concordance of radiology reports with oncology records | ||
| Text-only radiology reports | Multimedia radiology reports | |
| Concordance on target lesion selection with oncology records | 52% | 78% |
| Overall measurement concordance with oncology records | 38% | 68% |
The differences were statistically significant for both target lesion selection concordance (p = 0.005) and measurement concordance (p < 0.0001).
"This [improved concordance] has two important downstream results," Folio said. "First, because oncologists determine therapeutic response (usually by RECIST 1.1), then it behooves radiologists to take more ownership of the measurements, with improved concordance with what matters clinically to the patients upfront (agreed upon target lesions on baseline exam). This also results in improved efficiency; oncologists and radiologists can spend less time consulting on measurement details, while spending more time on more traditional, intellectual clinical-radiological consultations."
Folio noted that the NIH Clinical Center has a core lab with radiologist assistants creating verified target lesion measurements. For those institutions seeking to adopt these types of multimedia reports, Folio also recommends establishing a close working relationship with PACS, RIS, and EMR IT experts and vendors.
Future plans
The NIH team is now investigating the compatibility of the multimedia reports with other vendors' imaging modalities and PACS software. This compatibility would ensure that measurement metadata will transfer securely and accurately, therefore minimizing the need for duplicated efforts such as, for example, having to enter data twice or having to remeasure lesions on exams from referral centers, Folio said.
The group hopes that more cancer teams will adopt the technique to minimize transcription errors that result from remeasuring, handwriting, and duplicate data entry.
"Exporting measurement data from the single source of truth -- the radiologist measurement -- will undoubtedly reduce transcription errors while drastically improving efficiency," Folio said. "We strongly believe that multimedia reporting is here to stay, at least for us at NIH."