More than 25% of outpatient CT and MR exams ordered by primary care physicians at a hospital in the state of Washington were inappropriate, according to a new study in the March edition of the Journal of the American College of Radiology.
Researchers at the University of Washington's Harborview Medical Center in Seattle found that 26% of elective outpatient imaging exams did not meet appropriateness criteria (JACR, March 2010, Volume 7:2, pp. 192-197). While the data are from just one facility, they're consistent with other findings across the U.S., and indicate that decision-support tools may be needed to curb inappropriate utilization of imaging services.
How appropriate are referrals?
Dr. Robert Bree and Dr. Bruce Lehnert reviewed referring physician requests and medical records from 459 consecutive nonurgent outpatient CT and MR exams requested from adult primary care clinics at Harborview over a six-month period. Bree and Lehnert used evidence-based appropriateness criteria from HealthHelp, a national radiology benefits management (RBM) firm in Houston -- criteria that are updated quarterly and monitored for consistency with the ACR Appropriateness Criteria, they wrote.
The clinics were part of an electronic medical record system, so Bree and Lehnert could access complete clinic notes from the visits before the dates on which the imaging studies were performed. In more than 90% of the cases, the clinical histories provided from primary care physicians didn't give enough information to evaluate whether the exam had been appropriate, so the team reviewed each patient's medical record as well.
"The history given by the referring physician was often incomplete," Bree told AuntMinnie.com. "So we looked at all the visits prior to the exam to get as much detail as we could."
Bree and Lehnert rated the studies as either appropriate or inappropriate; they did not track how many studies for each test might have been recommended if there had been peer-to-peer physician conversation. Exam outcomes were placed into four categories:
- Negative results
- Positive results with incidental findings
- Positive results with findings related to the clinical problem that affected clinical management
- Positive results with findings related to the clinical problem that did not affect clinical management
Of the 459 outpatient CT and MR exams performed between June and November 2007, 284 (62%) were CT and 175 (38%) were MR. Bree and Lehnert found 341 (74%) of these exams to be appropriate and 118 (26%) to be inappropriate, based on information found in the patients' medical records.
The researchers found the highest level of inappropriate exams (62%) for brain CT studies without contrast, primarily done for nonacute symptoms and without any neurological findings. Other high percentages of inappropriate exams were CT maxillofacial (36%), CT spine (53%), MR spine (35%), and MR shoulder (37%).
Outcomes of the exams using report results and medical records showed that in the appropriate study group, 68 (20%) had negative findings, while 199 (58%) had positive findings and affected subsequent patient management.
In contrast, in the inappropriate study group, 55 (47%) had negative results, and only 15 (13%) had positive findings and affected management. The difference was highly statistically significant, according to Bree and Lehmert. Also for this latter group, 20 studies, or 17%, had positive findings, but these findings did not affect patient management; this included patients with complicating factors for back pain or headache. For many of these patients, Bree and Lehnert wrote, at their next visit the imaging exam results weren't discussed or the symptoms had resolved on their own.
Outcomes of imaging for appropriate and inappropriate examinations
|
|||||||||||||||
| Table courtesy of the American College of Radiology. |
The results weren't surprising, Bree told AuntMinnie.com: In fact, they're consistent with other studies across the U.S. Why? For a number of reasons, including the fact that primary care doctors don't have much time with patients, patients are asking for more imaging tests themselves, and the payment system primary care doctors work under makes ordering tests attractive.
"Our results aren't unique," he said. "They could probably be generalized across the country. Due to decreasing reimbursements for the cognitive specialties, primary care doctors are pressured to increase productivity and RVUs. A visit can generate a higher level of complexity if an imaging test is ordered. In the current climate, there are few disincentives to ordering an imaging exam."
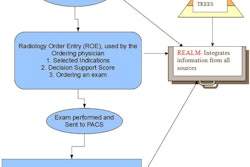
The study further bolsters the idea that clinical decision support would be a helpful tool for referring doctors, according to Bree: When decision-support tools are tied in with electronic medical records (EMR) and computerized physician order entry (CPOE), the culture of how tests are ordered and why begins to change.
"We're a ways from there," Bree said. "Only about 10% to 15% of physicians in the U.S. are using EMR, and fewer than that use CPOE. But we felt our study was an opportunity to show exactly where the baseline is and what can be done to improve."
By Kate Madden Yee
AuntMinnie.com staff writer
March 1, 2010
Related Reading
CDC report: MRI, CT, PET use spikes in physician offices, ER, February 18, 2010
Studies spotlight high CT radiation dose, increased cancer risk, December 14, 2009
NEJM study: Imaging procedures, radiation growing, August 26, 2009
MedPAC: Self-referring docs use more imaging, June 23, 2009
Study shows CT use has increased, diagnostic yield has not, March 3, 2009
Copyright © 2010 AuntMinnie.com