When performed within 12 hours of a patient coming to an emergency department (ED) with chest pain, adenosine stress cardiac MRI is valuable for the "safe, quick, and accurate" diagnosis of significant coronary artery disease, according to a study published in the April issue of Radiology.
The researchers from Duke University Medical Center concluded that stress cardiac MRI was the strongest predictor of significant coronary artery disease, and that patients fared well after the scans. For example, all patients with normal findings on cardiac MRI left the ED with an excellent prognosis and experienced no adverse events during a mean follow-up period of 14 months (± 5 months).
A comparison of stress cardiac MRI and stress echocardiography showed that both modalities performed well with respect to specificity and accuracy, with stress cardiac MRI having an advantage in sensitivity. The study was led by Dr. John Heitner from the Duke Cardiovascular Magnetic Resonance Center (Radiology, April 2014, Vol. 271:1, pp. 56-64).
Cardiac ED visits
It's estimated that more than 8 million people each year go to emergency departments with chest pain, according to the authors. The challenge for ED personnel is to identify those who are at increased risk for future cardiac events due to coronary artery disease.
Previous studies have found that approximately 3% to 5% of patients with acute myocardial infarction or unstable angina are mistakenly discharged from an emergency department. The result all too often is death. Therefore, prompt stress testing and diagnosis can play a critical role in patients with chest pain.
Stress echocardiography can achieve sensitivity of 75% to 80% and specificity of 85% to 90% for detecting coronary artery disease, according to past research. In addition, a negative stress echocardiogram is a reliable indicator of survival: The incidence of death is less than 1% per year among individuals with negative results.
As Heitner and colleagues noted, cardiac MR with adenosine stress perfusion imaging has also been shown to accurately diagnose coronary artery disease in various clinical settings. "However, data concerning the value of stress cardiac MRI in patients seen in the ED is limited, particularly in comparison with other stress modalities and in the early hours after presentation," they wrote.
Therefore, Heitner's group recruited patients who were seen in the emergency department for chest pain between October 2002 and December 2003 and were believed to have intermediate risk for coronary artery disease. The study cohort included 60 individuals with a mean age of 55 years, and 55% were women.
Intermediate risk was defined as having one or more coronary artery disease risk factors for men older than 40 years or women older than 50 years, or two or more risk factors for men older than 30 years or women older than 40 years.
Cardiac imaging protocol
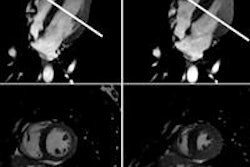
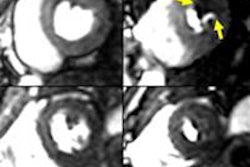
Stress cardiac MRI exams were conducted on a 1.5-tesla scanner (Avanto, Siemens Healthcare) with phased-array receiver coils. The protocol included four scans: cine imaging with the patient at rest to assess left-ventricular function; adenosine gadolinium first-pass imaging to assess stress perfusion; a repeat of first-pass imaging without adenosine at least 15 minutes later to assess rest perfusion; and delayed-enhancement imaging to determine myocardial infarction.
All patients also underwent stress echocardiography; the stress cardiac MRI and stress echocardiography exams were performed in random order within 12 hours of the individuals coming to the emergency department, the authors wrote.
Two experienced readers provided clinical interpretations immediately after the stress tests and blinded evaluations months later. For the blinded interpretations, cardiac MR images were placed in random order.
The researchers attempted to reduce the potential for reader bias by adding cardiac MR images from 60 other patients who were not enrolled in the study as part of the random review. Blinded readings were done twice, weeks apart.
Patients were considered to have significant coronary artery disease if angiography showed greater than 50% narrowing, or if death or a heart attack occurred during follow-up, Heitner and colleagues wrote.
'Uneventful' follow-up
Of the 60 patients, 14 had abnormal results on one or both of the imaging tests during the immediate clinical interpretation. These patients were admitted to the hospital and underwent invasive coronary angiography.
The remaining 46 patients were discharged from the ED and monitored for at least six months for follow-up clinical events. During that time, two patients reported recurrent chest pain and underwent additional cardiac tests; both were found to have normal coronary arteries at angiography. None of the patients died, had a heart attack, or were found to have significant coronary artery disease during the follow-up period.
"Thus, all 46 patients who had negative findings at clinical interpretation of both stress cardiac MR images and stress echocardiograms had an uneventful follow-up, and we determined they had true-negative findings for significant coronary artery disease," the authors wrote.
Stress cardiac MRI and stress echocardiography were similar in terms of diagnostic performance, according to the researchers. Cardiac MRI had higher sensitivity in the clinical and blinded interpretations, though the difference was not significant in the blinded phase.
| Diagnostic performance of imaging tests | |||||
| Modality | Sensitivity | Specificity | Accuracy | Positive predictive value | Negative predictive value |
| Immediate clinical interpretation | |||||
| Stress cardiac MRI | 100% | 92% | 93% | 67% | 100% |
| Stress echocardiography | 38% | 96% | 88% | 60% | 91% |
| Blinded interpretation | |||||
| Stress cardiac MRI | 88% | 90% | 90% | 58% | 98% |
| Stress echocardiography | 63% | 92% | 88% | 56% | 94% |
Diagnostic performance between the two stress imaging tests did not change significantly when the researchers changed the definition of significant coronary artery disease to narrowing of more than 70%, rather than 50%.
| Diagnostic performance with narrowing > 75% | |||
| Modality | Sensitivity | Specificity | Accuracy |
| Stress cardiac MRI | 100% | 91% | 92% |
| Stress echocardiography | 43% | 96% | 90% |
Adverse events
All patients tolerated the stress cardiac MRI procedure well. During imaging time of less than 50 minutes, there were no adverse events or complications associated with the use of adenosine. Stress echocardiography also was not associated with any adverse events, whether a treadmill or pharmacological stress was used.
"The main finding is that a cardiac MRI protocol incorporating adenosine stress perfusion imaging is safe, quick, and accurate when performed within 12 hours after presentation," Heitner and colleagues concluded.
Stress cardiac MRI was the strongest predictor of significant coronary artery disease and offered "performance characteristics that were similar to, if not better than, those of stress echocardiography," they added.
The authors did note limitations to the study, including its relatively small sample size, the fact that different stress methods were used for cardiac MR and echocardiography, and that newer cardiac MR and echocardiography technologies may produce different results.
"The potential for improvement in test sensitivity over that provided by stress echocardiography will require further evaluation in a larger population," they wrote.