The fabled Mediterranean diet may be good for your brain as well as your waistline. MRI has revealed that people who adhere to the diet have reduced brain white-matter hyperintensity volume, thus reducing their chance of chronic small-vessel damage, according to a study in the February issue of Archives of Neurology.
The Mediterranean diet typically includes a relatively high intake of fruits, vegetables, monounsaturated fat, fish, whole grains, legumes, and nuts. It also advocates moderate alcohol consumption and low consumption of red meat, saturated fat, and refined grains.
While previous research suggests the Mediterranean diet can reduce the risk of coronary heart disease, stroke, and cognitive disorders, the study authors asserted that no studies had been done to determine how the diet would affect the volume of white-matter hyperintensities.
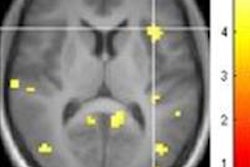
As markers of chronic small-vessel damage, white-matter hyperintensities are associated with vascular risk factors, including smoking, diabetes, and high blood pressure. White-matter hyperintensities also correlate with small-vessel damage in other organs, such as the eye and kidney, and can predict an increased risk of stroke and dementia.
"Although diet may be an important predictor of vascular disease, little is known about the possible association between dietary habits and [white-matter hyperintensities]," lead author Hannah Gardener, ScD, from the University of Miami Miller School of Medicine, and colleagues wrote (Arch Neurol, February 2012, Vol. 69:2, pp. 251-256).
The prospective study enrolled subjects with no history of stroke, who were 40 years and older and who had resided in northern Manhattan for three or more months. The participants were contacted randomly by telephone and asked questions about their dietary patterns during the previous year. Of the 1,091 participants, diet data were available for 966 people, who then were included in the study.
The researchers used a 10-point scale (0 to 9) to score participants' adherence to a Mediterranean diet, with higher scores indicating higher levels of adherence. Patients were then scanned with a 1.5-tesla MRI scanner (Philips Healthcare) to quantitatively measure white-matter hyperintensity volume. Gardener and colleagues calculated the association between the Mediterranean diet score and white-matter hyperintensity volume as a proportion of total cranial volume.
The researchers found that each one-point increase in a participant's Mediterranean diet score correlated with significantly lower white-matter hyperintensity volumes -- and, thus, the likelihood of chronic small-vessel damage. For example, participants who scored from 0 to 2 on the Mediterranean diet scale had a mean white-matter hyperintensity volume of 0.87, while those with diet scores of 6 to 9 had a mean volume of 0.63, indicating a lower level of hyperintensities relative to total cranial volume.
The results suggest a "possible protective association between increased consumption of a Mediterranean diet and small-vessel disease," Gardener and colleagues concluded. "The associations with [white-matter hyperintensity volume] may be driven by the favorable ratio of monounsaturated fat consumption over saturated fat."
The findings could also help explain recent studies that have linked consumption of a Mediterranean diet with lower incidence of neurological conditions such as mild cognitive impairment, Alzheimer's disease, and dementia -- areas where small-vessel damage could play a role. The authors recommended future studies to replicate and further explore a possible association between a Mediterranean diet and white-matter hyperintensity volume.
|
Study disclosures The research was supported by grants from the National Institute of Neurological Disorders and Stroke, a grant from the American Heart Association, and the McKnight Brain Institute. |