The sooner a person with a traumatic brain injury (TBI) undergoes an MRI scan, the better the chances of finding microbleeds in the brain, according to a study of military personnel published online September 15 in Radiology.
Researchers used susceptibility-weighted MRI (SWI-MRI) to evaluate 603 military personnel with TBI at Walter Reed National Military Medical Center. They found that nearly a quarter of the patients had evidence of cerebral microhemorrhages within three months of their injury, but the number with detected bleeds fell in the months afterward.
Cerebral microhemorrhages can result from TBI and lead to severe secondary injuries, such as brain swelling or stroke, so the ability to detect them early is paramount.
"The ability to monitor the evolution of microhemorrhages could provide important information regarding disease progression or recovery," wrote lead author Wei Liu, DSc, and colleagues (Radiology, September 15, 2015).
Incidence of TBI
As many as 1.7 million people in the U.S. experience traumatic brain injury each year, according to the U.S. Centers for Disease Control and Prevention's (CDC) National Center for Injury and Prevention Control. In addition, the Institute of Medicine estimates that 20% to 23% of military service personnel sustained TBI while serving in Afghanistan or Iraq.
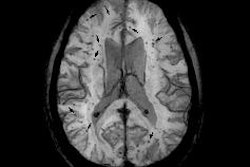
Traditionally, MRI with a T2-weighted gradient-recalled echo (GRE) sequence has been used to determine the number, severity, and size of cerebral microhemorrhages following TBI. However, past research has shown that SWI can provide better sensitivity than GRE, the authors wrote.
For this study, Liu and colleagues recruited military service personnel between March 2011 and November 2013. They included men and women between the ages of 18 and 60 years who had a clinical diagnosis of TBI. They excluded individuals who had metal implants or shrapnel, or a history of severe neurological or psychiatric conditions.
The majority of patients (559/603, or 93%) had mild cases of TBI, and 43 (7%) had at least one cerebral microhemorrhage. In addition, cerebral microhemorrhage was identified in 13 (23%) of 55 patients with follow-up images.
All exams were conducted on a 3-tesla scanner (Discovery MR750, GE Healthcare) using a 32-channel phased-array head coil. The MRI protocol included high-spatial-resolution anatomic T1-weighted and T2-weighted imaging, as well as four functional MRI sequences, diffusion-tensor imaging, contrast-enhanced perfusion imaging with dynamic susceptibility, spectroscopic imaging, GRE, and multiecho gradient-echo imaging.
The researchers also utilized an MRI technique known as quantitative susceptibility mapping (QSM) to measure iron concentration in the cerebral microhemorrhages.
SWI vs. GRE
Two radiologists independently reviewed the results and agreed on the findings in 41 (95%) of the 43 patients with microhemorrhages. With SWI, they detected 585 microhemorrhages in 37 patients, compared with 362 microhemorrhages at GRE imaging.
SWI also detected significantly more cerebral microhemorrhages per patient (17.7 ± 20.7) than GRE (11.0 ± 12.6). Most microhemorrhages (451/585, or 77%) appeared more conspicuous on SWI than GRE images, and the greatest number of microhemorrhages were found in the frontal subcortical regions (174, or 30%), followed by the parietal subcortical region (87, or 15%) and the temporal subcortical region (79, or 14%).
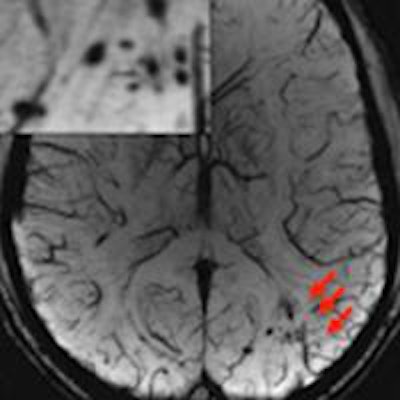
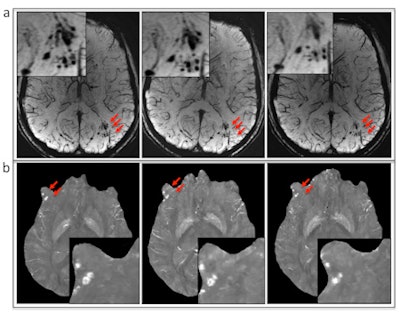 (A) Susceptibility-weighted MRI and (B) quantitative susceptibility mapping show the evolution of microbleeds (arrows) in a patient who had follow-up imaging. Image courtesy of RSNA.
(A) Susceptibility-weighted MRI and (B) quantitative susceptibility mapping show the evolution of microbleeds (arrows) in a patient who had follow-up imaging. Image courtesy of RSNA."Even though previous studies have shown that SWI is superior to GRE in the detection of hemorrhage, its clinical application in military clinics is still limited," the authors noted. "Our results indicate that for the identification of the presence or absence of cerebral microhemorrhages, SWI should be the method of choice clinically."
Additionally, the sooner an injured solider received an MRI, the greater the chance of finding cerebral microbleeding. SWI detected microhemorrhages in 24% of patients who underwent imaging within three months after their injury, compared with 18.4% for those scanned after three to six months, 7.6% for those scanned six to 12 months later, and 5.2% for those scanned more than a year later. The effect could be due to changes in iron deposits in the brain over time, making it more difficult to detect the microhemorrhages, according to the authors.
The situation is problematic, as the median time between head injury and the MRI scan in the current study was 856 days. The researchers attributed the interval to the fact that most traumatic brain injuries occur during remote military action where there is no access to a scanner.
Better access to MRI in the field could improve the detection of TBI, according to study co-author Dr. Gerard Riedy, PhD, chief of neuroimaging at the National Intrepid Center of Excellence at Walter Reed.
"Early characterization of cerebral microhemorrhages may help to explain clinical symptoms of acute TBI and identify the severity of brain damage," Riedy said in a statement. "We believe that having access to MRI in the field would facilitate early detection of TBI, thus providing timely treatment."