In a clinical trial inspired by the growing breast density awareness movement, researchers from Washington, DC, found that breast-specific gamma imaging (BSGI) is effective at identifying cancer in women of all breast densities, according to a paper in the February issue of the American Journal of Roentgenology.
The findings are good news, especially because more than half of women younger than 50 and at least one-third of women older than 50 have heterogeneously dense or extremely dense breast tissue, the group from George Washington University wrote.
"Improving breast cancer detection in women with dense breasts is important because of the decreased sensitivity of mammography in this population," wrote lead author Dr. Lauren Rechtman and colleagues. "MRI, which uses a physiologic approach to breast cancer detection, has been established as a useful adjunct breast imaging modality because of its increased sensitivity compared with ultrasound and mammography and its effectiveness in women of all breast densities. ... BSGI now offers those women who cannot or will not undergo MRI an alternative for physiologic imaging."
Rechtman's group evaluated the sensitivity of BSGI for detecting breast cancer in women with dense and nondense breasts. They found that the technology was comparable in both tissue types (AJR, February 2014, Vol. 202:2, pp. 293-298).
 Dr. Rachel Brem.
Dr. Rachel Brem.The Breast Imaging and Intervention Center at George Washington University has been using BSGI for more than 10 years on women who are newly diagnosed with breast cancer and those at high risk for the disease. The center performs at least four BSGI exams per day, corresponding author Dr. Rachel Brem said.
"Since an increasing number of states are passing breast density notification legislation, we wanted to know if BSGI was just as sensitive in women with dense breast tissue as in women without," Brem told AuntMinnie.com.
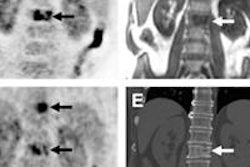
The study included 341 women with biopsy-proven breast cancer diagnosed from January 2004 through August 2009 who underwent BSGI before surgical excision. Rechtman's team classified women with predominantly fatty or scattered fibroglandular breast tissue (BI-RADS density 1 and 2) as nondense and those with heterogeneously dense or extremely dense tissue (BI-RADS density 3 and 4) as dense. BSGI exams showing focal increased radiotracer uptake in the area of biopsy-proven cancer were classified as positive.
BSGI identified 331 of 347 biopsy-proven breast cancers, for an overall sensitivity rate of 95.4%, the researchers found. The technology identified 136 of 142 breast cancers in women with nondense tissue, for a sensitivity rate of 95.8%, and 195 of 205 cancers in women with dense tissue, for a sensitivity rate of 95.1%.
Twenty of the 347 breast cancers, or 5.8%, were not identified by mammography; five of these were in nondense breasts and 15 were in dense breasts. Of these, BSGI detected all five cancers in women with nondense tissue (100% sensitivity) and 14 of 15 in women with dense breasts (93.3% sensitivity).
| BSGI performance by breast density type | ||
| Characteristic | Nondense breasts | Dense breasts |
| Pathologic subtype | ||
| Infiltrating ductal carcinoma | 97/100 (97%) | 127/133 (95.5%) |
| Ductal carcinoma in situ | 23/26 (88.5%) | 46/50 (92%) |
| Invasive lobular carcinoma | 8/8 (100%) | 4/4 (100%) |
| Other | 8/8 (100%) | 4/4 (100%) |
| Nuclear grade | ||
| Low | 26/29 (89.7%) | 29/29 (100%) |
| Intermediate | 60/62 (96.8%) | 84/91 (92.3%) |
| High | 48/49 (98%) | 78/80 (97.5%) |
"This study corroborates others that have shown that BSGI can detect mammographically occult breast cancer, although our study now shows that BSGI can detect mammographically occult breast cancer equally well in women with dense and nondense breasts," Rechtman and colleagues wrote.
BSGI vs. MRI
How does BSGI compare to MRI? BSGI costs less, takes less time to interpret, and is available to more women, according to the authors. However, BSGI does require a low-dose radiotracer, while MRI does not.
The radiation exposure is worth it, though, according to Rechtman and colleagues. Their study used a dose of 20 mCi to 30 mCi of technetium-99m sestamibi; now, George Washington University staff routinely use a lower dose of 7 mCi to 10 mCi.
"In the correct population, [the radiation dose] is a reasonable trade-off for early breast cancer detection," the authors concluded.
Further studies should compare the sensitivity and specificity of BSGI in women with dense and nondense breasts in a multi-institutional screening population. But BSGI definitely shows promise, according to Brem.
"This study further solidifies our clinical practice impression that BSGI can find breast cancer in any woman," she said. "We find this technology to be very exciting."