Will nuclear breast imaging technologies like positron emission mammography (PEM) become part of mainstream screening and diagnosis practice? Yes, but more hard data are needed, and radiation dose must be reduced, according to a presentation given at the recent National Consortium of Breast Centers (NCBC) meeting.
Dr. Michael Linver from X-Ray Associates of New Mexico offered session attendees at the Las Vegas meeting an overview of breast imaging technologies and a status update on nuclear breast imaging modalities, particularly PEM.
"There's a sophisticated imaging platform for molecular imaging, so with the molecular tag and isotope, it's possible that, in the future, we could accurately image and treat breast cancer at the same time," Linver said. "Stay tuned."
PET versus PEM
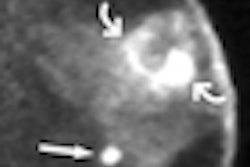
"We now have more experience with PET imaging and breast cancer," Linver said. "Since this technology is for whole-body imaging, it works well for staging breast cancer outside the breast. But PEM may be useful for primary breast cancer imaging."
Both PET and PEM are functional imaging technologies, and both use FDG. Whole-body PET provides images with 5-mm to 6-mm resolution and costs between $2 million and $3 million per scanner, Linver said. By contrast, PEM is optimized for small body parts, provides 1-mm to 2-mm resolution, and costs about $850,000.
MRI versus PEM
PEM is also more specific when compared with MRI and appears to have better sensitivity for ductal carcinoma in situ (DCIS), Linver said. He cited a recent study that included 388 women with newly diagnosed breast cancer. All of the women underwent MRI and PEM. Of the known cancers, MRI found 379 (98%) and PEM found 365 (94.5%) (Radiology, January 2011, Vol. 258:1, pp. 59-72). Of the 116 additional cancers found, MRI identified 60% and PEM found 51% (26% on MRI only; 17% on PEM only).
But the positive predictive value (PPV) of MRI was 53%, while the PPV of PEM was 66%, Linver said.
"MRI and PEM had comparable breast-level sensitivity," he said. "MRI's sensitivity was higher at lesion level than PEM. But PEM had a higher specificity."
PEM's value should be evaluated in the context of MRI's advantages and disadvantages, Linver said. MRI imparts no radiation and offers excellent anatomic detail, but it carries the risk of side effects from gadolinium, lacks specificity in hormonally stimulated dense breast tissue, and is expensive.
PEM has distinct advantages, as well, according to Linver.
"PEM shows glucose uptake in cancer cells," he said. "It's expensive -- about $1,500 -- but not as much as MRI. It's not affected by hormonally stimulated dense breast tissue, and there tend not to be significant reactions to FDG."
The technology does have its drawbacks in that it is also fairly expensive, lacks supportive data, and imparts a sizable dose of radiation to patients, according to Linver.
"The current radiation dose of all nuclear breast imaging tests is too high for annual screening," he said.
BSGI/MBI versus PEM
As for breast-specific gamma imaging (BSGI) and molecular breast imaging (MBI), which use gamma camera technology rather than PET, there are indications that PEM is comparable, Linver said. Like BSGI/MBI, PEM works well with premenopausal patients, or those using hormones; it helps to evaluate indeterminate areas seen on either mammography or ultrasound; it can evaluate multiple suspicious lesions to help with selecting a biopsy target; and it can be used for patients for whom MRI is indicated but not possible.
What are the advantages of BSGI/MBI as compared to PEM? BSGI/MBI is much cheaper than PEM or MRI and offers most of the advantages of these technologies. But their resolution is not as good as PEM, they are often affected by hormonally stimulated dense breast tissue, and they also use high doses of radiation.
PEM going forward
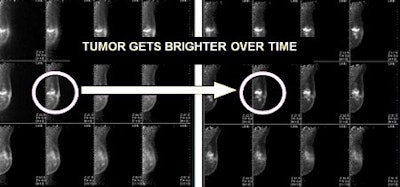
The future of PEM could be dual-time-point imaging: imaging at 90 minutes postinjection and then again at 210 minutes postinjection, as the tumor gets brighter over time, Linver said. Also in the near future could be a dedicated PEM/CT scanner for breast imaging.
What's the takeaway message with all these technology comparisons? Save PEM for diagnostic use rather than screening, Linver said.
"Mammography, ultrasound, MRI, tomosynthesis, dedicated breast CT -- all are safe for breast cancer screening, even when performed annually beginning at age 40," he said. "But right now, BSGI/MBI and PEM should not be used for routine screening at their current recommended dosage levels. These technologies are better for diagnostic purposes."