PET can provide strong indicators of overall and disease-free survival among patients with locally advanced non-small cell lung cancer (NSCLC) receiving radiation therapy, according to a study published in the February Journal of Nuclear Medicine.
Researchers from MD Anderson Cancer Center at the University of Texas found that higher residual standardized uptake values (SUVmax) on PET scans acquired after radiation therapy signal poorer overall and disease-free survival for NSCLC patients. In addition, a greater decrease in SUVmax in the lesion with the highest SUVmax at diagnosis resulted in longer overall and disease-free survival.
The researchers, led by Dr. Jose Lopez Guerra from the facility's department of radiation oncology, concluded that SUVmax readings on PET could help identify patients who are at high risk of recurrence and could lead to more appropriate treatment for these patients (JNM, February 1, 2012, Vol. 53:2, pp. 225-233).
The retrospective study reviewed MD Anderson's database of patients who were treated for lung cancer with radiochemotherapy between January 2007 and December 2008. The researchers included patients who had undergone FDG-PET both before and up to 3.5 months after completing radiation therapy. The final 49 participants had no history of thoracic surgery or radiation therapy, had no history of cancer, and had received a total radiation dose of 60 Gy or more.
Pretreatment FDG-PET scans were obtained a median of 26 days before the start of radiation therapy. The median time between the end of the radiation therapy and the FDG-PET evaluation was 2.5 months, ranging from one to 3.5 months.
Imaging protocol
For patients who had received adjuvant chemotherapy, the post-treatment scan was obtained after chemotherapy. PET/CT scans (Discovery ST, GE Healthcare) were started after a six-hour fast with an intravenous injection of 370 MBq to 555 MBq of FDG.
One experienced radiologist reviewed FDG-PET images and calculated the SUVmax for all 49 patients. The SUVmax in the gross primary tumor and in each lymph node was calculated and recorded from the scans obtained before and after radiation therapy.
The group found that for primary tumors, a higher SUVmax after radiation therapy correlated with shorter overall survival and disease-free survival. Subjects with an SUVmax less than the median of 3.7 had better overall survival and disease-free survival than those with an SUVmax of 3.7 or greater.
Guerra and colleagues also compared SUVmax after radiation therapy in patients who underwent PET scans 2.5 months or less after radiation therapy (the median time between the end of radiation therapy and the PET scan) with SUVmax in those who were evaluated more than 2.5 months after radiation therapy. They found no significant difference in SUVmax after radiation therapy between the subgroups.
"However, we did find that for the subgroup with the PET scan more than 2.5 months after radiation therapy, the SUVmax after radiation therapy was associated with overall survival time," the authors wrote.
In the review of SUVmax for regional lymph nodes, because some patients had more than one positive lymph node, the study analyzed the regional lymph node with the highest SUVmax and the SUVmax sum of all PET-positive lymph nodes separately.
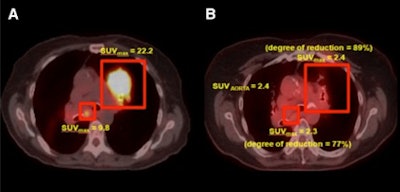 |
| PET/CT scans of FDG uptake by a primary tumor and lymph nodes at diagnosis (A) and after radiation therapy (B). Images courtesy of the Journal of Nuclear Medicine. |
The results showed no significant difference in the extent of SUVmax reduction between the primary tumor and the regional lymph node with the highest SUVmax after radiation therapy. However, after radiation therapy, the higher the SUV uptake in the single lymph node with the highest postradiation therapy SUVmax, the shorter the overall and disease-free survival times, the authors wrote.
In analyzing SUVmax for a target lesion -- either the primary tumor or regional lymph nodes -- the target lesion with the highest SUVmax at diagnosis was the primary tumor in 67% of cases and a lymph node in 33%. In these cases, a higher postradiation therapy SUVmax of a single target lesion also reflected shorter survival time.
SUVmax measurements after therapy for the primary tumor and lymph nodes, as well as the extent of reduction after radiation therapy in the target lesion that had the highest SUVmax at diagnosis, were associated with overall survival and disease-free survival in patients with NSCLC, Guerra and colleagues concluded.
"These findings indicate that the postradiation therapy SUVmax and the extent of reduction may become a routinely used, quantifiable, and analytic indicator of disease activity and treatment efficacy," they noted.