Using proton MR spectroscopy and PET, researchers from the Mayo Clinic in Rochester, MN, have identified significantly high levels of amyloid-beta deposits and other abnormalities in cognitively normal people with early signs of Alzheimer's disease, according to research in the August 24 online issue of Neurology.
The researchers found that individuals with high levels of amyloid-beta deposits also tend to have high levels of brain metabolites such as choline, which reduce cognitive skills, regardless of the amount of amyloid-beta deposits in their brains.
"In this population base of cognitively normal people, we found that 33% of them have high amyloid-beta load in their brain. That means they have Alzheimer's-related pathology in their brain," said lead study author Dr. Kejal Kantarci, an associate professor of radiology in Mayo's division of neuroradiology. "We are very curious to see what the future holds for these individuals who already have amyloid pathology in the brain, but they are normal at this point."
The study enrolled 311 patients from the Mayo Clinic Study of Aging (MCSA) from January 2009 through September 2010. MCSA includes adults in their 70s and 80s who do not have dementia. As part of the study, the enrollees undergo a series of neuropsychological tests and MRI/MR spectroscopy exams every 15 months.
The researchers excluded people who do not want to participate, and omitted others for safety reasons, such as patients with pacemakers and those with mild cognitive impairment.
MR spectroscopy's contribution
The researchers used proton MR spectroscopy to measure certain brain metabolites that are relevant to neurological diseases. Many of these metabolites are found to be abnormal in people with mild cognitive impairment and dementia, according to previous research, including one previous study by Kantarci and colleagues.
"We hypothesized that these biochemical abnormalities also are present in cognitively normal people who have preclinical dementia pathologies," she said. "That's why we investigated the biochemical changes in the brain that are associated with cognitive performance. We found that the worst abnormalities are, the worse the cognitive performance is."
Specifically, 3-tesla MR spectroscopy looked into the posterior cingulate gyri, the region of the brain that appears to reflect the earliest signs of abnormality and deals with functions such as memory, language, and visual-spatial functions.
"There are other regions of the brain that also are potentially important for memory function, but we chose that region because in our previous studies we found it to have more reliable spectra," Kantarci said. "Also, the reliability and reproducibility of that MR spectroscopy examination is much better in the posterior cingulate gyri than other regions of the brain."
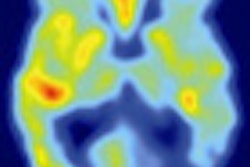
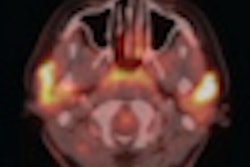
PET and PiB
Researchers also used PET imaging (DRX, GE Healthcare) with carbon-11 Pittsburgh Compound B (C-11 PiB) to assess the level of amyloid-beta deposits in the brain, which have been associated with early signs of Alzheimer's disease. The participants were also given tests of memory, language, and other skills.
The researchers found that 33% of these cognitively normal people had high levels of amyloid-beta in their brains. The chemical abnormalities identified by MR spectroscopy also correlated with the amount of amyloid-beta deposits.
"So, we think that both MR spectroscopy and amyloid load is pointing to the fact that there are individuals who are cognitively normal, but harbor significant amounts of Alzheimer's disease pathology in their brain," Kantarci concluded. "It also is causing a decrease in cognitive performance in these individuals, even though they are within normal limits."
Researchers also discovered a correlation between higher PiB retention and abnormal levels of choline in the brain. Previous Mayo Clinic studies have found choline elevation in people with mild cognitive impairment, with a majority of these individuals progressing to dementia, Kantarci noted.
While there are several possibilities as to why choline levels may be elevated, the role of choline in mild cognitive impairment or dementia is unknown. "What we need to do is more correlation studies to look at the pathological signatures and correlate that with imaging findings," Kantarci said. "No such study has found a correlation between choline and any of the pathological underpinnings of dementia."
Clinical relevance
By identifying imaging markers for preclinical dementia-related pathologies, researchers hope to develop tools to identify individuals who would benefit from preventive intervention before they become cognitively impaired.
"We don't have such treatments at the moment, but if and when those treatments happen, there has to be a way to identify those individuals who would benefit most from those treatments. For that we need imaging markers," Kantarci said. "Once those treatments are available, we need to evaluate those treatments in clinical trials and we need markers to tell us whether they are working or not."
Kantarci and colleagues plan to follow the participants in the study to determine whether cognitively normal individuals who have biochemical abnormalities, lower cognitive performance than their peers, and high amyloid-beta in their brain are at greater risk of developing dementia.