California researchers have developed a quantitative index based on functional brain data from PET scans to predict with a high degree of accuracy whether people with mild cognitive impairment (MCI) will progress to dementia within three years.
Researchers from the University of California, Los Angeles (UCLA) developed the Dementia Prognosis Index (DPI) software as a way of quantifying information derived from PET scans and improving the modality's ability to predict whether a patient will develop Alzheimer's disease.
Study results showed that the PET-derived DPI scores provided more conclusive information for half of the participants in a group whose initial PET scans were indeterminate. Among those whose prognostic status changed, 77% were deemed likely to develop dementia. Conversely, among those whose scans remained indeterminate, only 21% progressed to dementia three years later.
How the index works
The DPI tool is designed to put a numerical value on the rate of functional and cognitive decline using baseline PET scans in brain regions known to deteriorate in cases of Alzheimer's disease, comparing them with normal regions that are spared from the effects of dementia.
UCLA has licensed the software to Syntermed, which makes it available as part of the company's NeuroQ software package. Version 3.6 of the software, which includes functions for analyzing both FDG and amyloid PET radiopharmaceuticals, received U.S. Food and Drug Administration (FDA) 510(k) clearance in May.
Individuals who have low DPI scores have a greater rate of change in their DPI results on functional activity questionnaires and, subsequently, have an increased chance of progressing to dementia. Conversely, subjects with higher DPI scores tend to have more consistent functional activity results and a reduced chance of developing dementia.
The researchers evaluated baseline FDG-PET brain scans of 146 people with mild cognitive impairment who were enrolled in the Alzheimer's Disease Neuroimaging Initiative (ADNI) and had at least three years of clinical follow-up. Patients were excluded if they converted to Alzheimer's disease at an earlier time point, according to co-author Nare Torosyan, a research coordinator from UCLA's David Geffen School of Medicine, who presented the results at this year's Society of Nuclear Medicine and Molecular Imaging (SNMMI) annual meeting.
Torosyan and colleagues divided the 146 MCI subjects into two groups: One group consisted of 65 people (rule-derivation group) and the second group included 81 people (test group). The rule-derivation group was used to determine the optimal DPI cutoffs for dichotomizing and trichotomizing the prognostic outcomes.
"Once we determined the DPI ranges that maximized accuracy in this group, we then applied this criterion to the independent test group," Torosyan explained. "So the two groups are both composed of MCI subjects, but the test group was not used in the formulation of the predictive rule. The higher accuracy achieved by deriving cutoffs in one group and applying them to an independent test sample exemplifies the robustness of our rule."
To quantify brain activity, the researchers utilized the NeuroQ software to calculate standardized regions of interest, measuring activity in 240 different regions of the brain and then clustering them into 47 different volumes. The software then produces a report with the subject's original brain scan, a template brain image with regions of interest outlined, and the metabolism in the posterior regions of the brain illustrated in 2D color.
','dvPres', 'clsTopBtn', 'true' );" >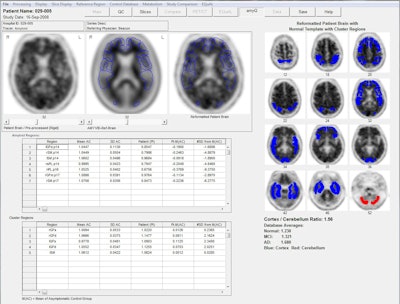
The software helped determine the DPI for regions of the brain adversely affected by Alzheimer's, such as the bilateral and posterior cingulate cortex and the bilateral temporal cortex, and compare the findings to regions of the brain not influenced by dementia.
Using this information, the researchers calculated ratios for the likelihood of subjects developing dementia within three years, classifying the results as high, low, or indeterminate risk.
"We defined conversion to dementia as anyone whose clinical rating increased from 0.5 at baseline to at least 1.0 at the end of the three-year time period," Torosyan explained. "These subjects were placed into a higher conversion-to-dementia or lower conversion-to-dementia category."
The researchers also established a category for subjects whose DPI was in a middle range, where the likelihood of progression to dementia could not be determined. In these patients, PET images were obtained one year after baseline scans and the risk of progression to dementia was reassessed.
What's the cutoff?
The researchers then calculated cutoff points, or numerical values on the DPI scale at which an individual might be considered to be at risk of converting to Alzheimer's disease.
Theoretically, the range of DPI scores can be as low as zero and as high as infinity. However, senior author Dr. Dan Silverman, PhD, from UCLA's department of molecular and medical pharmacology, said DPI results typically range from slightly greater than 1.0 to slightly less than 1.5.
"Human metabolism on a region-by-region basis [in the brain] revolves around such a tight [DPI] number that it doesn't take a very big deviation to accurately reflect an abnormality related to a disease," Silverman added.
For example, in their study, the analysis determined that subjects with a DPI greater than 1.2684 were considered at lower risk of converting to dementia, while those with a DPI less than 1.2684 were considered at greater risk of conversion.
When the researchers added in the middle-range group of so-called indeterminate subjects, they found that individuals above a DPI cutoff point of 1.2876 were even less likely to develop dementia, while subjects with a DPI of less than 1.2488 had a considerably greater chance of progressing to dementia.
The effect of the cutoff points on risk stratification can be seen in the MCI group, Torosyan said. For MCI subjects, 64% had DPI scores that could determine if they would progress to dementia (the "determinate" group); these patients were equally divided between high and low risk of progression. The predictions were accurate in 87% of cases based on three-year clinical follow-up data.
"This effect is even more dramatic in the [normal] group," she added. "We can see a significant amount of the nonconverters falling into the lower-risk conversion category, with only a few of the converters falling into this [lower-risk] category."
Similarly, only a few individuals who did not develop dementia fell in the high-risk DPI category, while a significant number of people who progressed to dementia were predictably in the high-risk area.
Prognosis accuracy
In evaluating the DPI results for the MCI and the normal groups, the index demonstrated sensitivity of 78%, specificity of 72%, and accuracy of 75%. In addition, positive predictive value was 71% and negative predictive value was 80%.
Among the subjects with initially indeterminate results, the totals were fairly even between converters and nonconverters within the upper and lower limits.
The researchers also found that the prognosis for 13 subjects remained indeterminate, with 11 (85%) of the 13 not progressing to dementia. Among 12 subjects whose DPI results changed their status to determinate, nine (75%) converted to dementia.
Among this group, the index achieved sensitivity of 85%, specificity of 87%, and accuracy of 86%. Positive predictive value was 85% and negative predictive value was 87%.
Based on the results, DPI enables PET scans of subjects with early MCI symptoms to be evaluated to predict whether conversion to dementia is likely to occur within three years, Torosyan concluded.
As for future research, Torosyan told AuntMinnie.com that she and her colleagues plan to add more patients from the ADNI database to the study and conduct more long-term follow-up.
"It would be especially interesting with the subjects [whose results] remained indeterminate to see what happens as we assess them again more than two years down the line," she said.