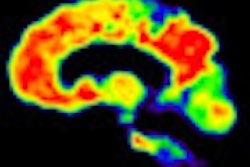
A task force assembled by the Society of Nuclear Medicine and Molecular Imaging (SNMMI) and the Alzheimer's Association has concluded that brain amyloid PET imaging could potentially help diagnose individuals with cognitive impairment if certain conditions are met.
These potential benefits could be realized when amyloid imaging results are combined with other clinical information and when the modality is performed according to standardized protocols by trained staff. The criteria were published online on Monday in Alzheimer's & Dementia and the Journal of Nuclear Medicine.
In addition, the Amyloid Imaging Taskforce (AIT) recommended that amyloid PET should be considered only after a comprehensive evaluation by a physician who is experienced in assessing and diagnosing cognitive impairment and dementia, and only if the presence or absence of amyloid would increase certainty in the diagnosis and alter the treatment plan.
The task force included dementia and imaging experts who reviewed scientific literature to develop a consensus on recommendations for the clinical use of beta-amyloid PET imaging.
As amyloid imaging becomes more prevalent in clinical settings, medical professionals must understand how to appropriately utilize the test, said SNMMI President Frederic Fahey, DSc, in a release announcing the criteria. Neurology and dementia experts should order the test only when appropriately indicated and nuclear medicine and molecular imaging professionals must ensure they have been adequately trained to interpret the results of the scan, he added.
Previous research has shown that increased beta-amyloid plaque is among the pathologic features associated with Alzheimer's. However, there are many older adults with normal cognition who have high levels of these plaques, so the potential clinical use of amyloid PET requires "careful consideration so that its proper role may be identified," AIT stated.
Potential candidates
According to AIT, appropriate candidates for amyloid PET imaging include those with persistent or progressive unexplained memory problems or confusion and who demonstrate impairments on standard tests of cognition and memory. In addition, individuals who meet requirements for possible Alzheimer's but who are unusual in their clinical presentation, along with those who have progressive dementia with an unusually early age of onset (before 65), are appropriate candidates for amyloid PET imaging.
Inappropriate candidates for amyloid PET imaging include those who are age 65 or older and meet standard definitions and tests for Alzheimer's, because a positive PET scan would provide little added value. Asymptomatic patients or those with a cognitive complaint but no clinical confirmation of impairment are also considered inappropriate for amyloid PET.
PET imaging should also not be used to determine the severity of dementia, or when requested solely on the basis of a family history of dementia or the presence of other risk factors for Alzheimer's, such as the APOE-e4 gene, according to the task force.
In addition, AIT discouraged use of the imaging technique as a substitute for genetic testing for mutations that cause Alzheimer's, as well as for nonmedical reasons, such as insurance, legal, or employment decisions.
How to do it
AIT suggested steps healthcare professionals can take when they do use amyloid PET. The group recommended the following:
- Evaluation by a dementia expert to assess the need for diagnostic testing, possibly to include amyloid PET if certain conditions are met
- Referral to a qualified provider of amyloid PET services
- Performance, interpretation, and reporting of the amyloid PET scan according to established standards
- Incorporating the PET result into the clinical assessment process
- Disclosure of the PET result by the clinician to the patient and caregivers and a discussion of the result and its management consequences
The panel also emphasized that amyloid PET results are not equivalent to a clinical diagnosis of Alzheimer's disease dementia. The imaging technique is only one option to manage patients, and it is not a substitute for a careful history and examination, AIT added.
Reimbursement status
The sensitivity and specificity of new radiopharmaceuticals for brain amyloid and the association between beta-amyloid accumulation and Alzheimer's suggest these new radiopharmaceuticals could aid the workup and diagnosis of patients with cognitive impairment, AIT concluded.
Currently, amyloid PET imaging is not covered by insurance and patients are generally responsible for the costs of the scan. PET costs can vary depending upon location, and other PET scans are known to cost between $1,000 and $3,000.
On January 30, the U.S. Centers for Medicare and Medicaid Services' Medicare Evidence Development and Coverage Advisory Committee (MEDCAC) is scheduled to hold a meeting to review policies regarding coverage of beta-amyloid PET studies.
Eli Lilly and its subsidiary Avid Radiopharmaceuticals are expected to draw much attention for their beta-amyloid PET contrast agent Amyvid, which received clearance from the U.S. Food and Drug Administration in April of last year.