The American College of Radiology criteria for determining appropriate imaging examinations is rapidly gaining favor among U.S. healthcare payors. The guidelines are credited with decreasing the costs associated with imaging self-referral by nonradiologists.
In fact, adopting the standards can result in millions in savings, according to data presented by an Israeli healthcare service that took up the ACR criteria for its organization.
"Our focus was to implement the CT and MRI utilization standards as a preauthorization program based on the ACR appropriateness guidelines," said Dr. Tal Sigal, chief radiologist and director of the nationwide imaging and quality control center for Maccabi Healthcare Services in Tel Aviv, Israel.
Sigal presented the results from her organization's adoption of the criteria at the 2004 RSNA meeting in Chicago. The goal of Maccabi Healthcare was to better utilize CT and MRI, improve the quality of care and imaging, and decrease the costs of CT and MR imaging, she said.
Maccabi Healthcare Services is the second-largest healthcare maintenance organization (HMO) in Israel, delivering primary care to approximately 1.7 million lives through more than 3,000 physicians, according to Sigal. In 2001, the provider conducted more than 12,000 MR exams and 84,000 CT exams, representing more than 1.4% of the HMO's total budget, she said.
The HMO initiated a program between July 2001 and December 2002 requiring authorization of CT and MRI requests at a preauthorization center staffed with board-certified radiologists, Sigal said. Since February 2003, all facilities in the HMO have participated in the now-obligatory program, she noted.
"Our recommendations (for CT and MR imaging use) are according to the ACR criteria and clinical radiological experience," Sigal said.
When a request for CT or MR imaging is submitted for preauthorization, there are three possible outcomes: authorization, with recommendation of modality and protocol; deferred, with a written explanation and telephone discussion with the referring physician regarding the decision; and disagreement, in which the referring physician can insist on an imaging study, according to Sigal.
"Where there is a physician and (preauthorization) center disagreement, CT may still be authorized by the referring physician, while MRI is available only after an appeal," she said.
After preauthorization was instituted, the number of CT and MRI examinations per patient decreased from 0.0151 and 0.0021, respectively, in 2000 to 0.0084 and 0.0020 in 2003.
The decrease in utilization of MR imaging between 2001 and 2003 was 8.7%, from 12,129 exams to 11,070 exams annually, she said. The adoption of ACR criteria for preauthorization saw a dramatic decrease in the utilization of CT imaging, which decreased 32.5% between 2001 and 2003, from 84,709 CT exams conducted annually by the HMO to 57,204 CT exams.
Sigal's team also compared the imaging costs of CT and MR exams between 2001 and 2003. Using the 2001 examination prices, $113 (U.S.) for CT and $500 for MR, the cost savings as a result of implementing the preauthorization process were approximately $3.12 million for CT and $553,000 for MRI, according to the researchers.
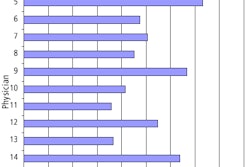
Her team also calculated the overall deferral rate by the preauthorization center and found that it ranged between 7.5% to 12.2% with a mean of 9.8% for CT, and 13.9% to 21.4% with a mean of 17% for MRI. Sigal noted that there was a variable effect in the deferral rates of the HMO's regional districts that was dependent on its cooperation with the preauthorization center.
"The higher the compliance of the district to the preauthorization policy, the higher the reduction in costs," she said.
On the basis of the group's research, Sigal said that preauthorization of CT and MRI examinations on the basis of the ACR criteria and clinical consultation results in more appropriate use of the modalities, decreases inappropriate radiation exposure to patients, and achieves a significant savings in imaging costs.
By Jonathan S. Batchelor
AuntMinnie.com staff writer
January 11, 2005
Related Reading
ACR to pitch Congress on 'designated physician imagers' for Medicare, January 6, 2005
Nation's largest insurer to adopt ACR criteria, accreditation, December 9, 2004
Radiologists (mostly) cheer as insurers set imaging rules, November 4, 2004
States, payors seek to stem tide of self-referral abuse, October 29, 2004
Stark II interim final rule leaves huge self-referral loophole, July 20, 2004
Copyright © 2005 AuntMinnie.com