
By this time, most people working in healthcare are aware of the October 1 deadline to begin using ICD-10-CM in place of ICD-9-CM for reporting diagnoses to Medicare. Healthcare Administrative Partners has previously posted information to help radiology practices prepare, and this new series of articles is designed to help radiologists fine-tune their documentation to ensure the best coding and uninterrupted reimbursement under ICD-10.
One of the major areas of concern for radiologists with ICD-10 is in the description of "pain" for proper diagnosis coding. A survey of historical coding by radiology practices showed that 17 of the 100 most commonly used ICD-9 diagnoses were related to pain.
Documentation requirements for pain
A few of the diagnoses related to pain -- such as unspecified chest pain, cervicalgia, lumbago, pain in thoracic spine, and backache -- match exactly with a single code under ICD-10; these will require no change to the current level of documentation being provided by the radiologist. However, most diagnoses will require a more specific description for the appropriate code to be applied. Documentation changes that will allow for proper coding of pain under ICD-10 are shown below.
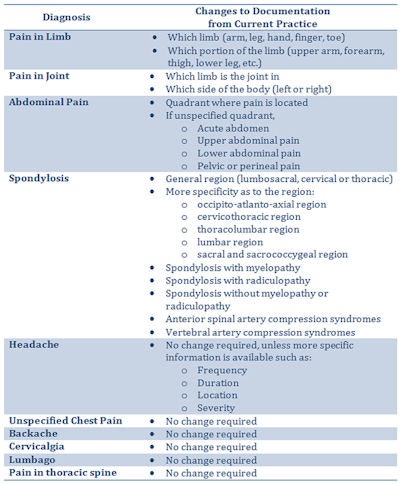

Image courtesy of Healthcare Administrative Partners.
Although "headache" is a one-to-one match from ICD-9 to ICD-10, a description of the additional information mentioned above could allow other more specific codes to be used. This type of information is currently not always available to the radiologist, and as a result the general nonspecific term will most commonly be used in radiology reporting.
Practice workflow considerations
With some revision of the practice's information-gathering system, more detailed information can be gained that will be useful for better coding and higher reimbursement. In the example of a headache diagnosis, the technologist can ask the patient at the time of the exam about the frequency, duration, location, and severity of the headaches. Modification of intake sheets or electronic medical record (EMR) templates will assist in this process, along with staff training on the new level of questions to ask.
Another potential source of additional information is the referring physician. Increased specificity should become a standard inquiry from radiology scheduling staff, and this request will most likely be understood by the referring offices, as they are in the midst of adapting to the same ICD-10 system. They will most likely have the information at their fingertips for their own diagnosis coding purposes; in fact, their diagnosis coding should be available for notation in the radiology group's records.
Conclusion
While Medicare is requiring that ICD-10 coding be used after October 1, 2015, it remains to be seen whether other insurance payors are able to accept the new system. The radiologist should always provide the coder with as much specific documentation as possible. This will maximize reimbursement regardless of the coding that is applied to the ultimate claim for payment of services.
Our next article will focus specifically on the proper documentation and coding of common fractures. Be sure to visit the Healthcare Administrative Partners website to receive the latest in this series of articles to help your radiology practice maximize reimbursement under ICD-10.
Carin Carlson is vice president of business development at Healthcare Administrative Partners (HAP), where she is responsible for all new business activity, including sales, marketing, product development, and strategic planning.
The comments and observations expressed herein are those of the author and do not necessarily reflect the opinions of AuntMinnie.com.



















