SAN FRANCISCO - The practice of defensive medicine among orthopedic surgeons is a significant factor in healthcare costs, contributing some $2 billion in unnecessary spending per year in the U.S., according to a study presented on Thursday at the American Academy of Orthopaedic Surgeons (AAOS) annual meeting.
Dr. Alex Jahangir of Vanderbilt University Medical Center and colleagues investigated the practice of defensive medicine by orthopedic surgeons in the U.S. and the resulting financial effects of such behavior. They found that 95% of orthopedic surgeons surveyed reported having practiced defensive medicine.
"Healthcare spending in American now is $2.3 trillion, or 16% of our GDP," Jahangir said. "This means that one out of every five dollars in this country is spent on healthcare, rather than education or infrastructure. And [politics clutter the issue]: It doesn't matter whether you're a Democrat or a Republican, if you take a dollar from education to pay for healthcare, you're still taking that dollar."
Defensive medicine is defined as medical practices that may protect physicians from liability without significant benefit to patients. Many studies have argued that defensive medicine is a major cost driver in healthcare, but the national prevalence of defensive medicine in the field of orthopedic surgery has not been investigated, Jahangir told AAOS 2012 session attendees.
The study data came from 2,000 orthopedic surgeons randomly chosen from the AAOS registry who received invitations to answer a Web-based survey on defensive medicine in September 2010. Of these, 61% (1,214) completed the survey. Jahangir's group performed a cost analysis using data from the U.S. Centers for Medicare and Medicaid Services (CMS), which were provided at the 2011 CPT code level and then aggregated to reflect the eight domains of care assessed in this study.
Of the 1,214 respondents, 95%, or 1,165, reported having practiced defensive medicine by ordering imaging, laboratory tests, specialist referrals, or hospital admissions, mainly to avoid possible malpractice liability. On average, 24% of all ordered tests were for defensive reasons, Jahangir said.
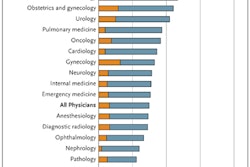
The group also broke out the percentages of particular tests that were ordered defensively:
- Radiography: 19%
- CT scanning: 26%
- MR imaging: 31%
- Ultrasound: 44%
- Referrals: 35%
- Laboratory tests: 23%
- Biopsies: 18%
Defensive hospital admissions averaged 7% each month, Jahangir said.
Defensive medicine can be "negative" -- that is, doctors can avoid treating high-risk patients in an effort to protect themselves from medical liability. Jahangir and colleagues found that 70% of their survey respondents had reduced the number of high-risk patients they saw over the previous five years.
Using the average national Medicare payment information from 2011 CPT code reimbursement data, the cost of defensive medicine per respondent was calculated to be approximately $8,500 monthly, or approximately $100,000 per year, which is roughly 24% of each physician's spending, Jahangir said.
Given the U.S. Department of Labor's statistic of 20,400 practicing orthopedic surgeons in the U.S., the group estimated that the national cost of defensive medicine for the specialty of orthopedic surgery is $2 billion annually.
Tort reform, practice protocols, or both?
"We asked our survey participants whether they would order fewer tests if there were true medical liability reform, and the majority said yes," Jahangir told session attendees.
But tort reform can only go so far, according to Jahangir: Clinical practice guidelines also need to be in place.
"A common problem orthopedists deal with is a patient presenting with knee pain," he told AuntMinnie.com. "So here's a doctor with 10 years of orthopedic training after college, and he examines the knee and diagnoses a bone bruise. Sure, there's a one in a million chance that the person has a cancer, and an MRI would pick that up, but it's probably not cancer. Clinical practice guidelines could protect that doctor from being penalized for not having ordered an MRI for the patient on the first visit, and allow him to make clinical judgments based on experience and evidence [rather than fear of liability]."