A new report published this week has harsh words for digital mammography, saying the technology was adopted due to heavy industry lobbying and is costing the U.S. Medicare system millions more than film-based imaging, despite an alleged lack of evidence that it's any better for older women.
The report was published on January 30 under the title "Unproven for Older Women, Digital Mammography Saps Medicare Dollars" by the Center for Public Integrity (CPI), a nonprofit research organization that specializes in investigative journalism. The article also was published in the February 7 issue of Newsweek under the headline "The Mammogram Hustle," as one of the first articles in a new content collaboration deal in which Newsweek pays CPI for exclusive articles.
The study claims that digital mammography has become the standard of care for breast screening for women older than 65 without clear evidence of its superiority to film-based imaging -- a situation that's been driven by higher reimbursement for digital imaging compared to analog mammography.
But breast imaging advocates believe the study only tells half the story, with the article glossing over a number of digital mammography's proven benefits. What's more, several mammography experts who were interviewed for the article felt the reporters approached the subject with an agenda -- to publish a follow-the-money exposé of a discipline that is actually one of the most cash-starved modalities in radiology.
"I think the article was incredibly irresponsible," said Etta Pisano, MD, dean of the College of Medicine and vice president of medical affairs at the Medical University of South Carolina in Charleston. "There are lots of things that Medicare is wasting money on, and digital mammography isn't one of them."
Digital's rapid rise
The article traces the rise of full-field digital mammography (FFDM), from when the U.S. Food and Drug Administration (FDA) approved the first system in 2000 to current times, in which 73% of all U.S. hospitals and clinics are using digital equipment. The article attributes the technology's rapid adoption to direct-to-consumer advertising campaigns that siphoned patients to breast centers with digital technology, while aggressive lobbying by mammography vendors resulted in higher reimbursement levels for digital procedures.
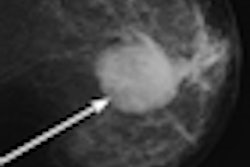
At the same time, the article claims that most clinical studies have failed to find any benefit for digital mammography versus film-screen in women older than 65, for whom Medicare pays for screening exams. The story bases its claims largely on the findings of the Digital Mammographic Imaging Screening Trial (DMIST) in 2005, which found that while FFDM might be better for younger women and those with dense breasts, it wasn't superior to film in older women -- and it's older women who have the highest breast cancer rates, the study points out.
The cost to the Medicare system of mammography's digital conversion has been dramatic, according to the article. Full-field digital mammography is reimbursed at a national rate of $129, compared to $78 for standard film mammography. And although the number of Medicare claims for mammograms fell between 2005 and 2008, the article states, the agency's expenses for mammography rose 17% to $636 million. The biggest jump in claims for digital mammography came after the DMIST results were released, the article states.
Mammography continues to be a favored child, the article claims, with the discipline sidestepping the painful reimbursements cuts that were meted out to other imaging modalities by the Deficit Reduction Act of 2005.
Mammography community responds
Reaction to the article by the mammography community has been swift. Mammography expert Gerald Kolb, who was quoted in the article, believes the authors, Joe Eaton, Elizabeth Lucas, and David Donald, approached the topic with a built-in bias against digital mammography.
Kolb, vice president of business development at mammography software developer Matakina International of Bend, OR, said he spent two hours on the phone with Eaton in two interview sessions, with the reporter approaching the topic "in an entirely negative way." The interview began with Eaton asking why digital mammography was used on older women for whom "there is no added benefit," and "asking if this wasn't just to make more money by overcharging Medicare."
"Eaton came into this subject with a bias," Kolb said in an e-mail to AuntMinnie.com. "I tried to teach, but I should have realized that the storyline had been written before the first interview."
Mammography vendor GE Healthcare has also fired back. The Chalfont St. Giles, U.K.-based vendor was highlighted in the story for its lobbying efforts in support of digital mammography, which included campaign contributions to U.S. congressional representatives, according to the article.
In a position statement released on January 31, GE said it "is proud of efforts to educate all people about the importance of digital mammography and to have urged the adoption of this important new technology when it was first introduced."
The company highlighted digital mammography's benefits in younger women as indicated by the DMIST trial, but it also pointed out that clinical trials in Norway and the U.K. have found that digital mammography has improved diagnostic accuracy for women of all age groups and breast densities. Digital technology has also been found to reduce radiation dose by up to 30%.
Finally, digital mammography confers benefits on providers, including higher diagnostic confidence and workflow benefits. "Digital mammography additionally improves access by providing radiologists with images from even remote locations and as such serves our rural communities," the company said.
Industry trade group Medical Imaging and Technology Alliance (MITA) of Arlington, VA, also disputed the article's contention that digital mammography was only effective in older women. The group cited a number of benefits behind the technology, including its lower radiation dose and workflow benefits, and the ease with which digital images can be incorporated into electronic medical records (EMRs) -- with EMR adoption being a major priority for the U.S. Centers for Medicare and Medicaid Services.
"Unfortunately, Newsweek’s story neglects these and other important facts about digital mammography," said Dave Fisher, executive director of MITA.
Inadequate reimbursement?
One of the most upset about the article is Pisano, the principal investigator on the DMIST study, who was quoted extensively in the version of the story that appears on the Center for Public Integrity's website. The article notes that when follow-on DMIST results were released in 2008, Pisano "told reporters that for most women there was no reason to seek out digital mammography because film was just as good." But now "Pisano has changed her mind" and recommends the technology, the article stated.
In speaking with AuntMinnie.com, Pisano believes the article's phrasing made it sound as if she changed her mind on a whim, when in actuality she became convinced of digital mammography's value due to technical advances in image processing that improved its performance and the peer-reviewed clinical studies that have come out since DMIST demonstrating FFDM's value.
These include a February 2010 article in the American Journal of Roentgenology that shows that FFDM has a 22% lower dose than film-screen mammography, a September 2010 study in Academic Radiology indicating that it shortens image acquisition times by 37%, and an article in the August 2009 edition of Radiology that suggests that digital mammography's improved performance was due to image processing that's only possible with digital.
But Pisano's main objection to the article was its characterization of mammography as a discipline awash with money that overwhelms the clinical judgment of practitioners. If anything, reimbursement for film-screen mammography was woefully inadequate during the analog era, and even now, the recent increases for digital imaging are barely enough to cover a typical breast center's costs.
"I'm stunned that this is the theme of the article, that radiologists are getting paid too much," Pisano told AuntMinnie.com. "You can call a plumber to your house and fix a toilet for more than Medicare pays for digital mammography."
By Brian Casey
AuntMinnie.com staff writer
February 2, 2011
Related Reading
Study finds USPSTF mammo guidelines would increase death rate, January 25, 2011
Medicare preventive coverage conflicts with experts, January 19, 2011
About half of eligible women fail to get mammograms, December 9, 2010
FDA's revision of FFDM rules may break market logjam, November 18, 2010
The breast screening hullabaloo: Where are we today? August 19, 2010
Copyright © 2011 AuntMinnie.com