The rise of new physician-extender professions like radiology practitioner assistants (RPAs) and radiologist assistants (RAs) is opening new doors for radiologic technologists. The new jobs offer upward mobility and greater job variety for many RTs, while new programs are springing up to train them. In the following article, RPA James Abraham describes his experiences.
A day in the life of an RPA begins days before many of the patients in our department even arrive at Kalispell Regional Medical Center in Kalispell, MT. My name is James Abraham -- I am a second-year RPA student through Weber State University, employed by Northwest Imaging with clinical rotation in radiology at Kalispell Regional Medical Center.
The RPA position is one of a few emerging physician extender positions that are becoming popular in medical imaging departments across the U.S. The position has been around since the mid-1990s, when the U.S. Department of Defense approached Jane Van Valkenburg, Ph.D., previous chair of radiologic sciences at Weber State University in Ogden UT, and asked her to create a program to train physician extenders for radiology.
The Weber State program is the only RPA program of its kind, and has grown steadily, with the number of accepted applicants doubling each fall semester over the last three years. While it is operated through Weber State University, the program has a strong physician base: physicians participate in the program, and each applicant has a radiologist preceptor. Although I have a specified preceptor, I am fortunate to have all the radiologists of Northwest Imaging available to support and instruct in my clinical preceptorship.
Click here to read supervising radiologists' views on the value of RPAs.The role of the RPA is multifaceted, and each radiology group tailors the position to match the needs of their practice. Many groups use RPAs in general radiology for heavy fluoroscopy schedules doing upper GIs, barium enemas, myelograms, lumbar punctures, and other procedures.
While I do some of those exams when needed, I am utilized more in the area of special procedures and interventional radiology. Many duties in special procedures revolve around the patient work-up for the procedure as much as the procedure itself.
Radiologists are bombarded many times each day with issues concerning pathways for patient care involving proper imaging, exams, and procedures. My goal is to create a higher standard of patient care while keeping the radiologists available and where they are most productive: in the reading room.
The RPA has not only helped in the area of performing exams and procedures, but also in the aspect of patient management. A typical day revolves as much around what is done for our patients before and after a procedure as it does when they are in our interventional suite.
In the past, a radiologist was intimately involved in approving and scheduling special procedures, taking up valuable time. Now, the vast majority of procedures are scheduled and followed up with limited radiologist involvement, many requiring essentially no radiologist input.
Our daily schedule is based on my prioritization of requested exams including, my triage of urgent/emergent cases with occasional radiologist input on a case-by-case basis. Our agenda today consists of one arteriogram, a CT-guided pelvic biopsy, an ultrasound-guided liver biopsy, a cholangiogram, three pre-MRI shoulder injection/arthrograms, a lumbar facet injection, a cervical selective nerve root block, a nephrostomy tube change, a potential dialysis fistula (to be worked in depending on what the Doppler ultrasound shows), plus the usual add-ons of any number of thoracenteses, paracenteses, PICC line placements, etc. Before our first patient arrives, the radiologist and I go over our entire schedule to formulate a game plan for the day and determine how I will be best utilized.
Unlike larger facilities or hospitals, the radiology department at Kalispell Regional Medical Center dedicates one radiologist to be responsible for the special procedures area. While our schedule may not seem overwhelming to some, our radiologist’s responsibilities are not limited to special procedures.
As volumes have increased substantially, the specials radiologist now helps read the hundreds of exams that pour into our facility via PACS from several outlying hospitals. My position as an RPA has decreased the amount of time the radiologist spends before, during, and after a procedure, while significantly improving our personalized care for our patients. The radiologist now splits his time between productive work in the reading room and physician-required time in special procedures. The result: optimum efficiency.
Among the cases on today's schedule, many were worked up several days in advance to facilitate the procedure. Someone must organize the lab values to be drawn, schedule the short-stay bed, review required imaging, check for appropriate equipment for the procedure, and arrange contact with the patient to give instructions.
Those who are scheduled for what is considered an invasive or major procedure are dealt with separately, from the time the referring office calls to schedule them until their discharge post-procedure. Today, patients for the arteriogram, CT- and ultrasound-guided biopsies, cholangiogram, and nephrostomy tube change all had advance work-ups to expedite everyone’s time. Postprocedural follow-up is just as important, and is the hallmark of a well-run specials department. With the exception of film review, these tasks are more cost-effectively performed, and I dare say better performed, by experienced physician extenders.
Depending on the procedure, I may work with a radiologist side by side, or autonomously under direct departmental supervision, meaning that the radiologist is available for any possible questions, assistance, or review I may require. Some procedures, such as simultaneous stent deployment for biliary reconstruction or synchronized "kissing" balloon techniques for iliac artery stenosis, require two sets of experienced hands. Conversely, a routine follow-up cholangiogram days after common duct reconstruction only requires the radiologist to review my images before the patient leaves the department.
The specials team
Our specials team typically consists of a radiologist, a nurse, a specials technologist, and me. My position is still split between technical duties for the hospital and RPA responsibilities for the radiologist. If the hospital is short-staffed, such as in the case of an arteriogram, then I must perform more in a hospital technical role rather than that of an RPA. This is both for patient safety and to help expedite our day.
In such situations I set up the suite for the arteriogram, then go to the holding area to get the patient’s consent and verify that all pre-procedure requirements are acceptable and within normal limits. Once the radiologist arrives I assist during the arteriogram.
After the areas of concern have been imaged and diagnosed, and depending on the type of arteriogram, I may finish imaging the remainder of the procedure while the radiologist confers with the referring physician. In this case I "ran" (imaged) the rest of the leg and unaffected side. Once it is determined that we have all of the necessary information, I hold pressure or close the puncture site with an approved closure device, and send the patient back to the holding room for later discharge.
The situation is similar for the biopsies. After I obtain consent, the patient is brought to the suite for imaging and localization. The radiologist is informed of our time frame, vital signs and medications are handled by our nurse per physician orders, and I begin localizing with anesthetic and place the biopsy guide needle. As position is confirmed, the radiologist makes any adjustments necessary and completes the biopsy. The patient is then sent back the holding room with post-procedure and discharge orders.
The follow-up cholangiogram, three pre-MRI shoulder arthrogram injections, lumbar facet injection, and tube change will all be handled similarly and according to the discussion the doctor and I had early this morning. If there are any discrepancies or differences when the patient arrives that differ from our earlier information, I inform a radiologist and adjustments are made as necessary. I help set up for the procedures, and unless there are any extenuating circumstances I perform the exams and procedures with supervision, confirmation, and finalization from the radiologist.
During the cervical nerve root block I function as technical staff for the radiologist. I do this for any procedure that Northwest Imaging feels would fall outside the acceptable scope of practice set by their group and the guidelines of Weber State University and the Certification Board of Radiology Practitioner Assistants.
Next, the ultrasound of the dialysis fistula shows increased velocity and decreased volume through the fistula, indicating a stenosis. This information is brought to the attention of the radiologist while we set up for a fistulagram. I consent and prep the patient for the procedure while the nurse begins monitoring.
I access the fistula with a micro access kit and perform a diagnostic fistulagram of the entire system, which reveals a stenosis at the venous outflow. The radiologist supervises and confirms the findings while preparing to angioplasty the stenotic area. After the procedure I hold pressure at the puncture site and, depending if sedation was used, the patient may be sent to the holding room for proper observation before discharge.
Today has been no different than any other day with the usual add-on cases. Today we had only one PICC line placement and a thoracentesis added to the schedule.
Routine PICC line placements and management are done by an outside service that contracts with our hospital, but when they cannot gain access they call radiology for an ultrasound-guided placement. This specific case was done portably in the ICU. After localizing the area, the radiologist is called to come to the ICU for verification of access. I wait until the last possible moment to call the radiologist, giving them as much time in the reading room and the least time standing in ICU as possible.
Once the radiologist arrives, placement is completed and the radiologist leaves while I finish the dressing. A portable chest x-ray is ordered for final confirmation of line placement, which the radiologist will see back in the reading room.
When our patient arrives for the thoracentesis we have already looked over the previous chest films and lab work. When everything is in order and before we proceed, I inform a radiologist that we are about to start a "thora" to be sure they are available. While I acquire consent from the patient our nurse applies the appropriate monitoring devices. I localize the effusion with ultrasound, prep the patient, and anesthetize the access point.
The radiologist arrives, I enter the pleural space, placement is confirmed, and aspiration is performed. The radiologist returns to the nearby reading room, but is available in case of any complications that may need to be addressed while the effusion is being aspirated. After the procedure is done, the patient receives a chest x-ray, which is checked by the radiologist and me before the patient leaves the department. Paracentesis procedures are performed in the same manner.
Between procedures I help with turning over the room, scheduling issues, filming, billing, and when feasible I do follow-ups on any patients in the hospital that have any drainages tubes. Dressing changes, output volumes, and possible follow up imaging will all be addressed when examining these patients. I will also check on our outpatients in our holding room to access them for post procedure discharge in conjunction with the radiologists’ written orders, other patients are called at home for follow-up as needed. Any concerns or questions from the holding room during a patient’s pre or post procedure care are usually brought to me. If necessary, then I go to the radiologist with any required issues. Again, my goal always being to improve patient care and maximize the radiologist’s time.
Our schedule is done and "A Day in the Life" moves toward its conclusion. I then look over tomorrow’s schedule for any possible red flags that we can address today if needed. As anyone in radiology knows, no matter how much pre-procedure work we put into a schedule, something can always slip by.
If a radiologist is available, preferably the radiologist assigned to specials the next day, we will start preparing our game plan and my role for tomorrow’s schedule. Everything I do for Northwest Imaging during my clinical internship is supervised to various degrees.
As I progress and eventually become certified, and as the radiologists become more comfortable, I anticipate near-complete autonomy for many of the routine exams and procedures I perform. I am grateful to Weber State, Northwest Imaging, and Kalispell Regional Medical Center for giving me the opportunity to be more than a "super-tech," and for maximizing my potential as a physician extender.
By James AbrahamAuntMinnie.com contributing writer
October 24, 2003
Related Reading
RTs are already tackling advanced tasks, survey says, August 15, 2003
New radiologist assistant position promises career boost for RTs, May 30, 2003
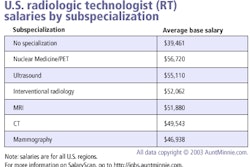
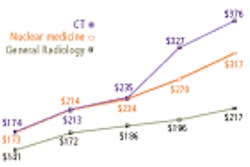
Survey reveals pay and perks for radiologic technologists, May 29, 2003
Breast center enlists radiographers for first look at mammograms, March 11, 2003
ASRT fund issues grants for RA programs, February 3, 2003
Copyright © 2003 AuntMinnie.com