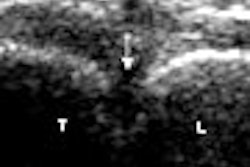
Ultrasound remains the key screening modality for patients with a higher risk of hepatocellular carcinoma, according to a presenter at the 2008 Gastrointestinal Cancers Symposium, sponsored by the American Society of Clinical Oncology (ASCO) and held in Orlando, FL.
"Hepatocellular carcinoma is becoming more common in patients with liver disease," said Dr. Eugene Schiff, chief of the division of hepatology and director of the Center for Liver Diseases at the University of Miami Miller School of Medicine in Florida. "Active hepatitis C virus infection with or without alcohol use accounts for most of the hepatocellular carcinoma in the United States."
"For patients at high risk of hepatocellular cancer, screening and surveillance with ultrasound should be conducted every six months," added Schiff, detailing some of the criteria of this at-risk population:
- Patients infected with hepatitis C virus and signs of cirrhosis
- Patients infected with hepatitis B virus without signs of cirrhosis
- Patients infected with hepatitis B and were raised in Africa or Asia where the virus is endemic
- Patients who consume large amounts of alcohol, which contributes to cirrhosis
- Patients who have other risk factors such as hemachromatosis or nonalcoholic fatty liver disease
Another screening option is alpha fetoprotein, but the test has a low positive predictive value (PPV) and a very low negative predictive value (NPV), Schiff said. Recent studies would bear out Schiff's assessment. According to a group from the All India Institute of Medical Sciences in New Delhi, ultrasound and triple-phase CT were useful for diagnosing hepatocellular carcinoma cases in patients with cirrhosis, while alpha fetoprotein turned in a low sensitivity of 25% (Oncology, December 13, 2007).
In a second study, investigators at the University of Barcelona in Spain found that contrast-enhanced ultrasound had a sensitivity of 51.7%, specificity of 93.1%, PPV of 93.9%, and NPV of 50.9%. The researchers also evaluated MRI in this patient population and determined that, if studies with both modalities are conclusive, then biopsy may not be necessary (Hepatology, January 2008, Vol. 47:1, pp. 97-104).
Among other imaging modalities, CT can be used to more clearly visualize the arterial system involved, while T2-weighted MRI will improve visualization of the tumor. Both should be seen as adjunct imaging tests to ultrasound, Schiff said. Liver biopsies, which are prone to hemorrhage, are unnecessary for most patients, especially if masses are seen in patients with a history of cirrhosis, he noted.
By Edward Susman
AuntMinnie.com contributing writer
February 12, 2008
Related Reading
Liver stiffness tied to portal hypertension in cirrhosis, May 16, 2007
Elastography noninvasively assesses hepatic fibrosis in HIV/HVC patients, February 7, 2006
Copyright © 2008 AuntMinnie.com