VANCOUVER - CT has long been the modality of choice for creating the simulations used in radiation therapy treatment planning. Now, however, a research team from the Washington University School of Medicine in St. Louis has found that fusion imaging provided by PET/CT may improve the accuracy of radiation therapy planning by decreasing errors caused by organ motion and deformation.
"CT has it own problems for sensitivity for certain kinds of cancer," said Dr. Sasha Wahab. "MRI is equally poor at defining the true extent of disease."
Wahab, from the department of radiation oncology at Washington University, shared his experience in utilizing PET/CT for simulation planning at this week's American Roentgen Ray Society (ARRS) meeting.
"Our concept was to incorporate biologic information to see if it could improve our ability to define target volumes," he said.
In the radiation oncology department at his institution, therapists use room-mounted positioning lasers to orient the patient in the treatment position and to build a custom immobilization device, Wahab said. This immobilization device, sculpted out of Styrofoam, is retained by the patient for the duration of treatment.
The team then conducts a traditional CT planning exam on the patient for backup redundancy and study comparison, according to Wahab. He noted that PET-guided radiation therapy (PGRT) has traditionally involved fusing diagnostic PET images with treatment planning CT images taken in the radiation oncology department, often from exams performed on different days.
"This process presented challenges for working with patients with cervical cancer because this introduced uncertainties caused by patient position variation, internal organ motion, and organ deformation," Wahab said. "We tried to decrease this uncertainty by using a PET and CT acquired during the same session."
The researchers believed that a CT performed at the time of PET/CT would have adequate spatial resolution for treatment planning and would allow more accurate image co-registration of PET and CT.
A simulation planning CT taken at the time of PET is no more accurate than the CT taken at a separate time, according to Wahab. The fact that the CT is obtained in the same session, with the patient in the radiation therapy treatment position and with minimal time interval between exams, makes the CT taken at the time of PET advantageous.
"By using a PET and CT taken back-to-back with the patient in the same treatment position, we reduce the risk of errors due to motion," Wahab said.
The PET/CT is taken at the institution's nuclear medicine department with the patient positioned in their customized immobilization device as though for radiation therapy treatment. An attenuation-corrected CT scan is taken, followed by a higher-resolution CT scan (120-150 mAs, 130 kVp, 3-mm slice thickness, 2.5-mm spacing, and a 480-mm field-of-view) through the region of interest, which is followed by a whole-body PET scan, Wahab said.
The datasets from the imaging studies are sent to a treatment planning system; although PET/CT image data are intrinsically co-registered, the planning software at Washington University requires that they be fused using applications built into that system, Wahab noted. These fused images are then used for contour delineation and treatment planning.
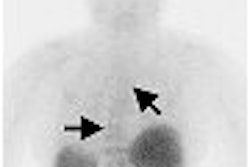
The researchers analyzed the results of 10 patients with cervical cancer who had radiation treatment planned using both a CT taken before PET and a single-session PET/CT. They found that PET/CT provided better correlation to patient anatomy than did a separate CT exam.
"Structures identified on the PET images demonstrate better spatial and volumetric correlation to patient anatomy on the CT taken at the time of PET than to patient anatomy on the traditional planning CT," Wahab said.
The PET/CT imaging protocol has been used successfully with more than 75 patients to date, and the radiation oncologists at Washington University have been very happy with the results of PGRT with PET/CT, he said. They have also reported more confidence in defining target volumes using the combination modality.
"The better we can see the tumor, the better we can treat it," Wahab said. "Using PET/CT to guide treatment planning, we can more effectively target cancer cells so that we can deliver higher radiation doses to the tumor and still spare the dose to normal tissue. This may lead to more effective treatment with lower side effects."
By Jonathan S. Batchelor
AuntMinnie.com staff writer
May 4, 2006
Related Reading
NEMA paper touts imaging's role in oncology, April 6, 2006
Carefully considered radiotherapy stymies endometrial cancer relapse, March 3, 2006
Subcutaneous amifostine feasible during radiotherapy for head and neck cancer, February 28, 2006
MRI-guided cancer treatment, February 1, 2006
Whole-body PET/CT efficiently stages colorectal cancer, January 3, 2006
Copyright © 2006 AuntMinnie.com