When computer-aided detection (CAD) technology is integrated directly into a PACS workstation and clinical workflow, it can significantly increase reader sensitivity for detecting lung nodules in thoracic CT exams, according to a study published online in the Journal of Digital Imaging.
A research team from Siemens Healthcare and NYU Langone Medical Center found that total interpretation time with the use of CAD as a second reader was less than four minutes for both newly credentialed and highly experienced chest radiologists.
"The integration of CAD into PACS increases reader sensitivity with minimal impact on interpretation time and supports such implementation into daily clinical practice," Luca Bogoni, PhD, Dr. Jane Ko, and colleagues wrote.
To date, the adoption and use of CAD systems to detect lesions and solid lung nodules on CT images has been burdened by the inconvenience of needing to use a separate workstation. Integration into a diagnostic PACS workstation would eliminate this workflow efficiency stumbling block, according to the authors (J Digit Imaging, June 19, 2012).
The guidelines on CT lung cancer screening published in May from the American College of Chest Physicians (ACCP) and the even broader guidelines published last week from the American Association for Thoracic Surgery (AATS) may also play a role. The anticipated increase in screening from these guidelines could spur adoption of lung CAD software that helps improve accuracy without compromising workflow performance.
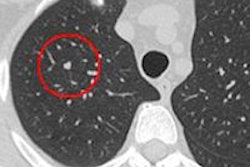
In their study, the researchers measured the efficiency and accuracy of five radiologists interpreting 43 contiguous 5-mm studies for solid, noncalcified lung nodules ≥ 3 mm in diameter. They first reviewed the chest CT images without CAD and then with CAD.
Following initial scan acquisition, CT images were simultaneously channeled to the hospital's PACS and a CAD server (syngo CAD Manager 2008B, Siemens). CAD software (syngo LungCAD, Siemens) processed the images, which were then sent as a separately labeled CAD series and incorporated with the CT exam.
For this set of exams, the CAD algorithm generated a total of 206 marks. A total of 134 true-positive nodules were included in 39 of the 43 chest CT exams. The mix included 50 nodules ≥ 5 mm, 35 nodules ≥ 4 mm, and 49 ≥ 3 mm. Four of the exams had no solid nodules larger than 3 mm.
Sensitivity gains
The use of CAD software significantly improved detection of solid nodules, regardless of nodule size. Its impact was more pronounced with respect to cases that had been identified as negative without the use of CAD, according to the researchers.
The group reported that the total time for readers to interpret each CT scan and evaluate CAD marks averaged slightly less than four minutes. The median time was 186 seconds, of which 143 seconds was for CT images without CAD.
"Measurement of the time taken to clinically utilize CAD proved acceptable, despite the need for readers to independently document all findings," the authors wrote.
On the downside, the total number of false-positive interpretations more than doubled when CAD software was used, from an average of 2.8 to 6.4 for the 43 cases. The individual case average was 0.7 without CAD and 0.15 with CAD.
"Similarly to prior studies, in nearly all cases CAD improved the sensitivity of reader's detection of solid lung nodules without an undue number of [false-positive] findings," the authors wrote.
A major source of inefficiency was localizing the proposed CAD marks on the original images. The researchers recommended adding an automated localization mechanism. They also acknowledged that it would be helpful to incorporate some of the advanced standard functionalities of a standalone CAD workstation into a PACS workstation.
The use of CAD in patients with diffuse lung disease or patients with easily identified multiple lung metastases is less promising, they also noted. How radiologists who are not chest specialists would perform remains to be determined, according to the researchers.
"While this study supports the use of CAD when restricted to studies in patients in whom identification of nodules is critical with a low pretest probability, use of CAD integrated with PACS clearly requires still further evaluation in more diverse clinical settings," they wrote.
Average sensitivity of radiologists and CAD to identify true positive nodules
|