CHICAGO - Patients who have a negative coronary CT angiogram after presenting at the emergency room (ER) for cardiac-suspected chest pain can safely be sent home, researchers reported at this week's American College of Cardiology (ACC) meeting.
There were no major adverse coronary events in the 30-day period after patients were discharged for a negative CT study for the chest pain, reported Dr. Harold Litt, PhD, associate professor of radiology at the University of Pennsylvania. The study was also published online March 26 in the New England Journal of Medicine.
The primary end point of the American College of Radiology Imaging Network (ACRIN) PA 4005 study was an event rate of less than 1% at 30 days for patients sent home after undergoing CT evaluation. The statistical confidence interval reached 0.57%, well within the 1% limit.
The findings also showed that receiving coronary CT angiography as opposed to standard of care for patients presenting in the ER for chest pain resulted in an increased rate of discharge from the ER and a shorter hospital stay, Litt said.
The study was funded by the Pennsylvania Department of Health, with additional funding from the ACRIN Foundation, which in turn receives funding from the U.S. National Cancer Institute.
"Patients presenting to the emergency department with symptoms of a potential acute coronary syndrome are a diagnostic dilemma," Litt said in his plenary presentation. He noted that many patients are admitted to rule out heart-related causes for chest pain, but few of these patients will actually have a cardiac diagnosis.
A coronary CT angiogram has a high negative predictive value for coronary artery disease, he added. He and his colleagues attempted to enroll enough patients to give the study sufficient statistical power to demonstrate an acceptable safety end point -- in this case, an event rate of less than 1% at 30 days.
Patients were eligible for the study if they were older than 30 years and exhibited signs or symptoms of potential acute coronary syndrome, but they did not show evidence of acute ischemia on electrocardiogram and needed admission or testing to exclude acute coronary syndrome.
The patients were evaluated using at minimum a 64-slice CT scanner and underwent contrast-enhanced CT angiography. Stress testing was allowed at the discretion of the local facility.
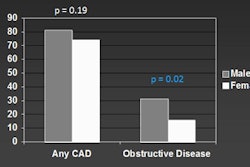
Between July 2009 and November 2011, 1,392 patients were enrolled in the trial; eventually, 908 patients were randomized to CT, and 462 patients received standard of care. Patients assigned to CT were about 49 years of age; those assigned to standard of care were about 50 years of age. There were slightly more women than men in the study, and approximately 60% of the patients were African-American.
About 16% of the patients assigned to CT did not receive the exam, leaving 767 patients. In 83% of the cases, the test showed coronary stenoses that were less than 50%, or a negative finding. Among the 462 patients assigned to standard of care, 58% were given stress tests, compared with 14% of those who underwent CT. Cardiac catheterization was performed in 4% of patients in each group.
Of the 640 patients who had negative CT examinations, no major acute coronary events occurred within 30 days, Litt reported. He also said that 50% of the patients in the CT group were discharged from the emergency department, compared with 23% of those receiving standard of care.
The average length of stay for the CT group was 18 hours, compared with 25 hours for those who received standard treatment (p < 0.001). The length of stay was 12 hours for those patients in the CT group who had a negative angiogram (p < 0.001).
When patients who underwent CT had results that indicated possible heart disease, fewer negative tests were performed and more diagnoses of coronary artery disease were made than among those undergoing standard treatment, Litt also said.
However, physicians should be careful in how they apply the study's results, especially for patients at higher risk of heart disease, according to Dr. Patrick O'Gara, professor of medicine at Brigham and Women's Hospital and Harvard Medical School. O'Gara moderated the plenary sessions at ACC and did not participate in the trial.
"This study looked at patients with low or intermediate risk of heart disease," O'Gara cautioned. "The results reported here cannot be extrapolated to patients in higher risk categories."