When clinicians need to image the abdominal aorta and the lower extremity arterial tree in patients with peripheral arterial occlusion disease (PAOD), matching the injection of contrast to when CT scanning begins in those regions is key.
Dr. Dominik Fleischmann, associate professor of radiology at Stanford University in California, has developed protocols for optimal wait times between contrast injection and the start of CT imaging based on how fast the bolus reaches the abdominal aorta or arterial tree. Fleischmann presented his findings at Stanford's 2006 International Symposium on Multidetector-Row CT in San Francisco.
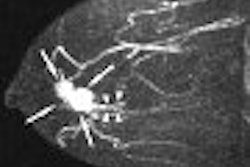
Patients with cardiovascular disease and limited cardiac output often have problems with arterial enhancement following contrast injection. The condition may lead to inadequate opacification of the abdominal aorta. "We know that the bolus transit down the peripheral territory can be substantially delayed in patients with occlusive disease," Fleischmann told attendees.
Of course, outrunning the bolus is a real problem with today's fast multidetector scanners. If imaging starts when contrast reaches the aorta, CT acquisition -- in Fleischmann's words -- "may in fact be faster than the bolus transit speed down the legs and feet." The question is whether clinicians can scan faster than the bolus travel time to the peripheral arterial tree.
Travel time
To find the answer, Fleischmann and his colleagues calculated the timing on 20 patients with PAOD by injecting a test bolus to measure time attenuation curves in the abdominal aorta. The results showed that the bolus took approximately 10 seconds to travel from the aorta, but the timing varied per patient, depending on the degree of PAOD. In some patients, travel time took only four seconds (177 mm/sec), while it took as long as 24 seconds (33 mm/sec) in other patients.
"What you can extrapolate from that is that it takes up to 48 seconds to fill the entire peripheral arterial tree, and you can inject five seconds shorter than your scan time," Fleischmann said.
From that starting point, clinicians can adjust injection and scan times accordingly. With an acquisition speed of 33 mm/sec, the risk of outrunning the bolus is very low. "If you have a speed of 6 mm/sec -- which you can easily achieve with a 16-row scanner -- you are probably scanning faster than the bolus moves down the aorta in about one-third of your patients," Fleischmann added. Using a 64-row CT with an acquisition speed of 19 mm/sec, a clinician would scan faster than the bolus travel time to the arterial tree in approximately 50% of the patients.
A head start
To solve the problem, Fleischmann recommends increasing the contrast media injection rate for the first five seconds of the injection, or increasing the scanning delay relative to the arrival of contrast media in the aorta, allowing more time for the contrast to enhance the aorta.
"You need to give the bolus a head start," Fleischmann explained. "Say the scan time is only 25 seconds. You wait until the contrast arrives in the aorta, then wait another 15 seconds and then catch up so that overall you are ready in 40 seconds when the contrast arrives from the aorta. This also very reliably gives you very bright arterial opacification, despite the presence of substantial arterial occlusive disease."
|
||||||||||||||||
When using a 64-slice CT scanner, Fleischmann said the protocol at Stanford is to slow down the system and scan for 40 seconds, regardless of the size of the patient. With a variable pitch setting and by alternating the CT tube current, this reduces radiation to the patient and provides reliable images across a wide range of patients.
By Wayne Forrest
AuntMinnie.com staff writer
September 28, 2005
Related Reading
New contrast injectors go with the digital flow, September 28, 2006
Grown-up decisions: When is MDCT the best choice in children? September 30, 2005
Part II: Palliative steps prevent contrast-induced nephropathy, September 20, 2006
Part I: Identifying patients at risk of contrast-induced nephropathy, September 13, 2005
Low-dose CT matches x-ray for pediatric sinus imaging, June 9, 2005
Copyright © 2006 AuntMinnie.com