Automated plaque assessment in coronary CT angiography (CCTA) is a promising new way to evaluate a patient's plaque burden quickly and noninvasively -- but it won't be quick or accurate without the use of advanced iterative reconstruction, according to researchers from Massachusetts General Hospital in Boston.
Automated techniques are still in their infancy, but once they become more reliable they promise to greatly improve risk assessment and management compared with, for example, calcium scoring, by precisely quantifying the amount of coronary artery plaque -- fibrotic, lipid core, and calcium -- that is present.
"We know the plaque volume and characteristics ... are at least as important as the presence of calcium," said Dr. Stefan Puchner in an interview with AuntMinnie.com. "If we could make plaque assessment more accurate, we could implement all this stuff in our daily practice."
The process isn't accurate today. Automated plaque quantification requires significant time for radiologists to fix the incorrectly drawn vessel wall boundaries, making it impractical for routine use. Manually drawing the boundaries would actually take about a day's work for each patient, so automation is the only way forward, Puchner said. The group wanted to determine if an advanced reconstruction algorithm might produce fewer errors and make semiautomated plaque estimation practical.
In a study that reconstructed ex vivo coronary vessel segments using three different reconstruction methods, the study team found that, indeed, accuracy in plaque quantification depended on the reconstruction algorithm, as well as vessel size and the extent of calcifications. Using advanced reconstruction, fewer corrections were needed to the vessel wall segmentation, Puchner reported at the 2013 European Congress of Radiology (ECR) in Vienna. Specifically, they compared the use of automated vessel assessment using model-based iterative reconstruction (MBIR, GE Healthcare) compared with an earlier IR algorithm, advanced statistical iterative reconstruction (ASIR, GE), or conventional filtered back projection (FBP) reconstruction.
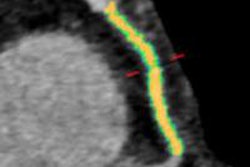
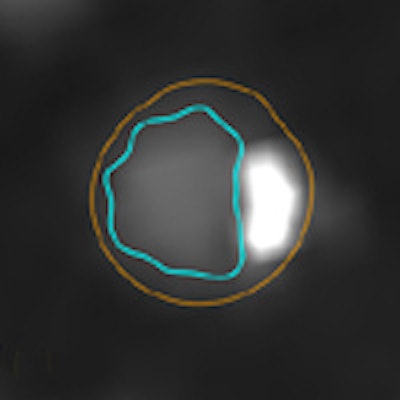
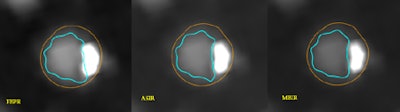
 Cross section of a noncalcified plaque reconstructed with the three different algorithms (left to right: FBP, ASIR, MBIR). No significant differences can be seen between the three algorithms in terms of correct delineation of the plaque borders. All images courtesy of Dr. Stefan Puchner.
Cross section of a noncalcified plaque reconstructed with the three different algorithms (left to right: FBP, ASIR, MBIR). No significant differences can be seen between the three algorithms in terms of correct delineation of the plaque borders. All images courtesy of Dr. Stefan Puchner.For subjects, the group examined three ex vivo human hearts imaged with CCTA and reconstructed with FBP, ASIR, and MBIR. An automated plaque quantification tool (Vitrea Cardiac Solutions, Vital) was applied to each of the three reconstruction algorithms to fit the outer and inner vessel wall boundaries in nine "triplets" constituting 27 vessels. Only the first 40 mm of the contrast-filled vessels was used for analysis.
Each coronary cross section for which the software assigned incorrect boundaries was tallied and corrected in a blinded manner. The group then compared the number of vessel wall corrections between the different reconstruction algorithms using a Chi-square test.
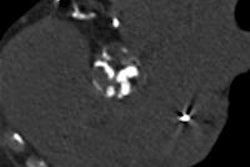
 Cross ection of a calcified plaque reconstructed with the three different algorithms (left to right: FBP, ASIR, MBIR). In this case, FBP shows an incorrect delineation of the inner vessel wall boundary, including parts of the calcified plaque. In contrast, the vessel wall boundaries in the cross sections reconstructed with ASIR and MBIR are correctly delineated by the software.
Cross ection of a calcified plaque reconstructed with the three different algorithms (left to right: FBP, ASIR, MBIR). In this case, FBP shows an incorrect delineation of the inner vessel wall boundary, including parts of the calcified plaque. In contrast, the vessel wall boundaries in the cross sections reconstructed with ASIR and MBIR are correctly delineated by the software."Our analysis included the percentage of corrections between the three algorithms, and a per-vessel comparison of the percentage of corrections between the three algorithms," Puchner said in his presentation.
In all, the study comprised 2,295 cross sections in 0.5-mm increments from nine coronary vessels, combined into 765 coregistered triplets evaluated with the three algorithms. Overall, 31% of the cross sections needed boundary corrections, he said. Outer vessel wall boundary corrections were needed in 400 cross sections, and inner vessel boundaries were needed in 381 cross sections.
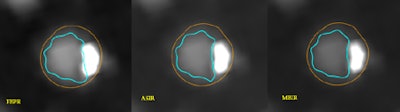
 Cross section of a calcified plaque reconstructed with the three different algorithms (left to right: FBPR, ASIR, MBIR). In this case, FBP and ASIR show an incorrect delineation of the inner vessel wall boundary, including the whole or parts of the calcified plaque. Only in the cross section reconstructed with MBIR are the boundaries correctly delineated by the software.
Cross section of a calcified plaque reconstructed with the three different algorithms (left to right: FBPR, ASIR, MBIR). In this case, FBP and ASIR show an incorrect delineation of the inner vessel wall boundary, including the whole or parts of the calcified plaque. Only in the cross section reconstructed with MBIR are the boundaries correctly delineated by the software.The percentage of corrected cross sections was lower for MBIR (24.1%) versus ASIR (32.4%, p = 0.0003) and FBP (36.6%, p < 0.0001) -- but the differences were only marginal between ASIR and FBP, he said.
"We found that MBIR works much better than the conventional algorithms ... significantly reducing the number of corrections needed compared to FBP and ASIR, whereas the difference between the two other algorithms was not significant," Puchner said.
The use of MBIR significantly reduced the need for vessel wall boundary corrections compared with other reconstruction algorithms, particularly at the site of calcifications.
Automated segmentation is certainly faster than manual processing, Puchner said. Just on the three cases used in the study and in the analysis of the proximal 40 mm of each vessel, use of the software saved about three hours compared with what manual segmentation would have required. There is significant processing time required to create MBIR reconstructions, he acknowledged, but in those cases, it's the technologists, not the physicians, who are spending the additional time, he said.
"The next step will be to look at it in an in vivo environment, to see this application in a beating heart," Puchner told AuntMinnie.com. And to test other applications and other iterative reconstruction schemes, of course.
"I'm pretty sure that the other newer algorithms will have similar effects, because overall some studies have shown that the use of newer algorithms reduces blooming effects and other stuff that makes it difficult for the software to delineate it correctly," he said. With manual segmentation, radiologists tend to overcorrect for older reconstruction algorithms and undercorrect for newer techniques, "but if the software does it, the software is much more dependent on image quality, and it makes a difference if it was reconstructed with the newer algorithms or the older algorithms."
Automated plaque measurements will also have to be compared with assessments in other modalities such as intravascular ultrasound, and even to histology using the donor hearts, he said.