BOSTON - New research presented at this week's American Society for Therapeutic Radiology and Oncology (ASTRO) meeting reveals that dynamic contrast-enhanced breast MRI may help clinicians determine whether mastectomy patients should also receive radiation therapy to the axillary lymph nodes.
With the increasing practice of staging chemotherapy before surgery and radiation therapy, the ability to accurately determine axillary nodal status (ANS) may be diminished, according to Dr. Christopher Loiselle, a resident at the department of radiation oncology at the University of Washington Medical Center in Seattle. He recommended that dynamic contrast-enhanced (DCE) MRI kinetics be investigated as a surrogate marker for traditional axillary staging for locally advanced breast cancer patients undergoing neoadjuvant chemotherapy.
Loiselle presented the findings of researchers from the Seattle Cancer Care Alliance and the University of Washington Medical Center in a poster presentation on Sunday at the ASTRO meeting.
The researchers wanted to determine the correlation between DCE-MRI kinetics of breast cancer and ANS and identify a kinetic pattern which could have prognostic value. They performed a retrospective review of their institutions' radiation oncology database, DCE-MRI database, and clinical and pathology records. Their patient population consisted of 167 patients with invasive breast cancer who received external-beam radiotherapy during a 22-month period from January 2006 through October 2007.
Of these 167 patients, 121 were excluded from the study because they received neoadjuvant chemotherapy prior to breast surgery, leaving a total of 46 patients who underwent surgical staging, either sentinel node biopsy and/or axillary dissection prior to the initiation of chemotherapy with DCE-MRI kinetic data. In this patient database, 30% were node positive and 70% were node negative.
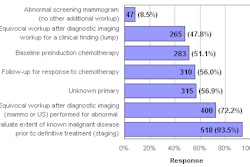
Kinetic values for initial peak enhancement (PE), percent rapid enhancement (RE), and percent washout (PW) were calculated for each patient's primary tumor using breast MRI CAD (CADstream, Confirma, Bellevue, WA). Kinetic parameters were analyzed according to whether the patient's ANS was negative or positive. Differences in PE, RE, and PW between the node-positive and node-negative groups were evaluated statistically with the Mann-Whitney U test.
The researchers determined that while there was no difference in the PW between the groups, both the PE of the primary tumor (p = 0.0027) and the RE (p = 0.0436) were significantly greater in node-positive patients than in node-negative patients.
Kinetic values for breast MRI
|
||||||||||||||||||||||||||||||||||||||||||||||||
"The findings of this study need to be replicated in future prospective studies," Loiselle said in an interview with AuntMinnie.com. "The ability to stage lymph nodes by evaluating the biology of the tumor through its characteristics as seen on a breast MRI has the potential to be more clinically accurate than performing exploratory lymph node surgery after chemotherapy."
"The ultimate benefit may be that some women can be spared radiation therapy, especially those with smaller tumors and tumors that have not spread to the lymph nodes," he said. "Patients who are node negative likely will not receive significant benefit from radiation after mastectomy, as long as they have a relatively small tumor and negative surgical margins. It would be of great benefit to them if they are spared the radiation dose to the chest as well as potential complications from axillary node dissection, such as pain, limited range of motion, and lymphodema."
By Cynthia Keen
AuntMinnie.com staff writer
September 22, 2008
Related Reading
Routine MRI at breast cancer diagnosis linked to treatment delays, September 9, 2008
Breast MRI gains momentum for screening high-risk women, September 2, 2008
The comprehensive breast center: Greater than the sum of its parts, September 2, 2008
Breast MRI develops role as surgical planning tool, September 2, 2008
Preoperative MRI helps detect additional breast cancer, but may delay treatment, July 25, 2008
Copyright © 2008 AuntMinnie.com