As mammography evolves to embrace new technologies, coders will need to grow along with it. Digital mammography and computer-aided detection (CAD) are two key technologies that coders are bound to encounter, if they haven't already.
"I think more and more facilities are starting to bill for digital mammography," said Stacie Buck, vice president of Southeast Radiology Management in Stuart, FL.
"Right now our facilities are billing for CAD; we don't have any sites that bill for digital mammography," she said. "But most providers do use computer-aided detection."
Proper documentation is critical when using these technologies, Buck said. According to the American College of Radiology (ACR), neither of these technologies is considered investigational, so facilities should not have too much trouble receiving reimbursement for them, she said.
Below is a basic outline of these new technologies, what they are, how they should be used, and how you should code them to avoid reimbursement denials and errors.
CAD
CAD is a technology designed to help catch potential breast cancers that may be missed by a radiologist. It works by highlighting potential problem areas on a digitized version of a mammogram. The radiologist then reviews those areas to determine whether there is a cancer that they might have missed. CAD has been shown to be effective in detecting some cancers that would have otherwise gone unnoticed, and is therefore becoming something of a standard of care in the industry.
However, a potential drawback of CAD is that it can highlight several normal areas on any given mammogram -- false positives -- that can lead a radiologist to dismiss the results too readily or cause physicians to order unnecessary biopsies and follow-up procedures.
Medicare reimburses CAD as a separate add-on payment when used with either film-based or digital mammography. However, the current procedural terminology (CPT) codes for CAD are different for diagnostic or screening mammography.
According to Medicare guidelines, facilities can report CPT code 76082 for diagnostic mammography CAD in combination with the standard mammography codes 76090 and 76091 (mammography, unilateral; and mammography, bilateral). They can also be reported with Healthcare Common Procedure Coding System (HCPCS) codes G0204 and G0206.
In addition, CPT 76092 and HCPCS G0202 can be reported along with 76083, which is the code for screening mammography. A new CAD code will be added starting July 1 to be used in conjunction with MRI codes, according to Buck.
The code is an add-on that will replace unlisted code 76498, which had been used to report this combination of procedures. The code was added onto MRI breast codes 76093, unilateral, and 76094, bilateral. The new code description is as follows:
0159T, computer-aided detection, including computer algorithm analysis of MRI data for lesion detection/characterization, pharmacokinetic analysis, with further physician review for interpretation, breast MRI. (List separately in addition to code for primary procedure.) Note: Use 0159T in conjunction with 76093, 76094.
Some payors will likely recognize this code and will pay it; others will not pay anything additional on it. No relative value units (RVUs) have been assigned by Medicare for this code. Therefore, payment comes at the payor's discretion.
It's crucial to ensure that your physicians are documenting whenever they use CAD so you can bill for it. If not, you will not be capturing these charges and will miss out on the payments.
Digital mammography
Since the release of the Digital Mammographic Imaging Screening Trial (DMIST) in September 2005, which showed that digital mammography is as good as and in some cases better at detecting cancers than film-based mammography, digital mammography has moved to the forefront.
Digital technology brings with it the advantages of increased productivity and reduced chemistry and film costs, but with its $400,000-plus price tag per unit, facilities may have a difficult time crossing the digital divide.
In addition to the capital expenditure, a digital system can cost up to $135,000 per year to operate. By comparison, an analog system incurs $24,000 per year in operating costs.
Therefore, ensuring proper reimbursement is critical for the increasing number of facilities that are adopting digital mammography equipment.
According to the ACR, full-field digital mammography (FFDM) should be covered because it is approved by the U.S. Food and Drug Administration and should be viewed no differently from coverage of digital fluoroscopy, chest x-ray, or angiography.
These modalities all converted to digital without changes in coding or reimbursement. In addition, the ACR's committee on coding and nomenclature recommends that if a private payor does not accept HCPCS G-codes, digital mammography should be billed using the CPT codes that are used for film mammography.
Documentation is also important when it comes to billing for digital. Be certain to include your certification number on the claim.
Failure to do this will result in an automatic denial, Buck said.
By Kelly Bilodeau
AuntMinnie.com contributing writer
July 13, 2006
The "Mammography Regulation and Reimbursement Report" is a 12-page monthly newsletter designed specifically for mammographic technologists and supervisors that is published by HC Pro. The periodical offers ideas for better practice management from peers, billing tips, MQSA regulatory updates and guidance, and business ideas related to breast imaging. For a free trial subscription, please click here.
Related Reading
Easing the pressure of compression for patients, June 27, 2006
Digital mammography: Can your facility afford to make the leap? May 11, 2006
MQSA reauthorization: What to expect and how to prepare, April 13, 2006
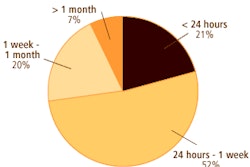
Increasing patient satisfaction seen in reduced wait times, March 28, 2006
Preparing for an MQSA inspection: Steps for a successful visit, March 2, 2006
Copyright © 2006 HC Pro