Virtual colonoscopy (VC or CT colonography [CTC]) using automated insufflation is as effective and safe in colon cancer patients with severely stenosing lesions as it is in the general population, according to a new study from Seoul, South Korea, and New York City.
"Recent studies have shown that automated CO2 insufflation significantly improves colonic distension compared with the manual method," wrote Dr. So Yeon Kim and colleagues. "Optimal colonic distension is one of the essential factors for successful performance of CTC. Recent studies have shown that automated CO2 insufflation significantly improves colonic distension compared with the manual method, particularly in the left colon, in screening and symptomatic patients."
Stenosing lesions narrow the diameter of the colonic lumen, sometimes to an extent that a colonoscope can't be maneuvered past it. There are case reports discussing the use of automated CO2 in patients with stenosing lesions, but the authors said they were unaware of studies consisting entirely of patients with stenosing colonic lesions. Therefore, they sought to determine the effectiveness of automated CO2 insufflation in a cohort of patients with severe stenotic lesions, and evaluate the safety of the method immediately after colonoscopy.
"CTC is not recommended shortly after colonoscopic polypectomy, particularly after snare polypectomy, or after biopsy because of the increased risk of perforation," they noted. "Automated pressure-controlled CO2 insufflation with its high safety profile and use of low infusion pressure, however, may possibly be safe even in patients who have recently undergone colonoscopic polypectomy or biopsy."
The research by Kim and colleagues from Asan Medical Center at the University of Ulsan College of Medicine in Seoul, with collaborators from Seoul University College of Medicine, and Weill Medical College of Cornell University in New York City, appears in the American Journal of Roentgenology (March 2008, Vol. 190: 3, pp. 698-706).
The study prospectively examined 74 consecutive patients (45 men and 29 women, mean age 56.3 ± 11.3 years) referred for newly diagnosed colon cancer or suspicion of colon cancer, all of whom had undergone conventional colonoscopy by one of five highly experienced gastroenterologists within eight days prior to VC.
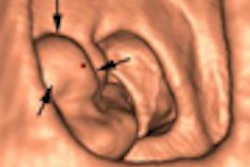
Colonoscopy was incomplete in 36 of the 74 patients due to severe luminal narrowing that prevented advancement of the colonoscope in the sigmoid or rectosigmoid colon (n = 25), descending colon (n = 1), and transverse colon (n = 4). Intolerance to pain prevented the completion of colonoscopy in two other patients, and colonoscopy was complete in the remaining 36 patients.
Virtual colonoscopy was performed following bowel preparation with a polyethylene glycol (PEG) solution (4 L, 246 mL of PEG) the night before conventional colonoscopy. Forty-three patients underwent optical colonoscopy and then VC, between one and four hours later, on the same day. Patients who underwent VC on a different day were prepped with a 250-mL magnesium citrate solution and 10-mg bisacodyl laxative. Prior to scanning, all patients underwent automated bowel insufflation with approximately 2 L to 2.5 L of CO2 (ProtoCO2l, E-Z-EM, Lake Success, NY) set at a maximum pressure of 25 mm Hg.
When insufflation was incomplete, the extension tube was checked to confirm the absence of blockage, and the rectal catheter was pulled back slightly to prevent blockage from the colon wall, the authors wrote.
"If unsuccessful, slight flexion of the patient's knee and hip joints to relax the abdomen, gentle manual palpation of the abdomen, and additional positional changes according to the location of the poorly distended segment ... were all attempted," Kim's group wrote. These maneuvers were performed in 34 stenotic patients and 38 of the nonstenotic patients.
Images were acquired on a 16-detector-row scanner (Somatom Sensation 16, Siemens Healthcare, Erlangen, Germany) at 16 x 0.75-mm collimation, and analyzed on a commercial workstation (AW version 4.2 with colonography, GE Healthcare, Chalfont St. Giles, U.K.) and reviewed by an experienced observer blinded to stenotic or nonstenotic patient group. Distension was graded on a four-point scale, with four being optimal.
The results showed that distension was not significantly different between stenotic and nonstenotic patient groups in any colonic segments, in both prone and supine positions. In stenotic patients, the mean distension of colonic segments proximal to the severe luminal narrowing was graded at 3.7 ± 0.7 and 3.8 ± 0.7 on the four-point scale for supine and prone positions, respectively, representing nearly optimal distension. Distal to the narrowing, the mean distension was 3.9 ± 0.4 and 3.8 ± 0.6 for supine and prone positions, respectively.
Likewise, the researchers found no significant difference in distension (p = 0.076) between patients who underwent same-day VC and those who had a separate bowel prep and VC within eight days of colonoscopy. Colonic perforation was not noted in any of the patients, including 65 who underwent same-day colonoscopy, which included 62 snare polypectomies, two polypectomies using biopsy forceps, and 63 routine mucosal biopsies. The mean diameter of the 78 lesions removed at colonoscopy (64 sessile and 14 pedunculated polyps) was 6.0 mm ± 3.7 mm (range, 1 mm to 20 mm). Interobserver agreement was excellent.
"The prevalence of synchronous cancer in patients with colorectal cancer is reported to range from 2% to 7.1%; therefore, preoperative evaluation of the entire colon in patients with colorectal cancer is widely recommended," the authors noted.
Limitations of the study included the lack of baseline CT to minimize radiation dose. This step would have served to identify any patients who were already perforated following colonoscopy.
In addition, although the end result of distension procedures was measured, evaluation of the entire insufflation process would have permitted the comparison of other factors, such as the amount of CO2 and the time required to achieve optimal distension.
"Automated pressure-controlled CO2 insufflation is as efficient in colonic distension for CTC in colorectal cancer patients with severe luminal narrowing as it is in patients without severe luminal narrowing," Kim and colleagues wrote.
By Eric Barnes
AuntMinnie.com staff writer
March 22, 2008
Related Reading
Automated CO2 insufflation edges patient-controlled air in VC, June 2, 2006
Automated CO2 insufflation maintains lead, December 30, 2005
Automated CO2 insufflation improves VC, December 1, 2004
Electronic CO2 insufflation beats air in virtual colonoscopy, March 12, 2003
Copyright © 2008 AuntMinnie.com