C-RADS, the virtual colonoscopy reporting system developed by the Boston-based Virtual Colonoscopy Working Group, is an efficient way to evaluate practice experience in virtual colonoscopy (VC or CT colonography [CTC]), and can be used to compare exam quality, readers, and patient cohorts, according to researchers from Boston.
Dr. Michael Zalis from Harvard University Medical School in Cambridge, MA, and Massachusetts General Hospital (MGH) in Boston presented the study at the 2006 RSNA meeting in Chicago.
The C-RADS reporting system offers a measure of global clinical significance for virtual colonoscopy reporting (Radiology, July 2005, Vol. 236:1, pp. 3-9).
The system includes a C score designating colonic findings in the aggregate exam (C0 negative exam, C1 continued screening, C2 VC surveillance or optical colonoscopy, C3 and C4 recommended for immediate resection), as well as an E score to classify extracolonic findings. The E score works similarly to the C score, ranging from E0 (inadequate exam) to the E3 and E4 designations, which recommend immediate follow-up of extracolonic findings.
"The purpose of our study was to assess the utility of C-RADS in the analysis of different (VC) clinical cohorts," Zalis said." We applied C-RADS scores to two different cohorts: one a heterogeneous clinical practice at my own institution (MGH), and secondly and retrospectively in a research screening cohort originally obtained at the Walter Reed Army Medical Center in Washington, DC."
The researchers calculated the distribution of colonic and extracolonic findings by site and reader experience (either more or less than 100 cases), Zalis said. In the subgroup of patients subsequently referred to optical colonoscopy (i.e., C-RADS C3 or C4), the researchers calculated the rate at which clinically significant polyps were confirmed as true positives at follow-up. Finally, the frequency of C-RADS scores and the likelihood of true-positive referral were calculated for both cohorts using contingency tables.
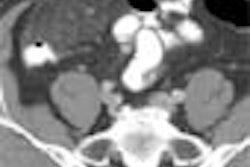
Both cohorts underwent low-dose thin-section VC after cathartic bowel cleansing, though there were differences. For example, the MGH group used automated CO2 insufflation and no fecal tagging, while the Walter Reed group had room-air insufflation and fecal tagging, Zalis said.
In the prospective MGH cohort, there were 334 patients (mean age 62, slight female predominance); 57 (17%) were for asymptomatic screening, 276 (83%) for symptoms, and 207 (62%) for failed colonoscopy. In this group, 37 of the 334 (11.1%) cases scored C3 or C4, and 89 of the 334 (26%) received E3 or E4 scores (further workup indicated). The Walter Reed subjects were younger, with a male predominance, and entirely asymptomatic.
For both cohorts, the results showed that "experienced readers were much more likely to have true-positive calls than inexperienced readers, and the difference was statistically significant," Zalis said. Clinically significant histology was confirmed in C3 and C4 cases interpreted by experienced readers at a rate of 94% (18/19) versus 67% (12/18) for inexperienced readers (p = 0.04).
"In C score distribution, for MGH we saw a predominance of C1 scores, as might be expected, with a smattering of C2 and C3," Zalis said. "Interestingly enough, higher C0 and C4 numbers were seen (in the heterogeneous MGH group). The Walter Reed cohort had a predominance of C1s and C2s, but a significantly lower number of C0s and C4s than the MGH group."
Overall, 8% of the cases in the Walter Reed screening cohort versus 10% of the heterogeneous MGH cohort were classified as C3 or C4 (p > 0.05); and 9.3% (screening) versus 27% (heterogeneous), respectively, were classified as E3 or E4; (p < 0.0001), he said.
"The analysis of these scores allowed us to change our referral patterns from our gastroenterology colleagues, as well as the interpretation of one of our radiology colleagues of what C0 stood for," Zalis said. "So there was a practical benefit of doing this study in terms of our own practice methods."
The limitations related principally to the use of two cohorts with slightly different VC acquisition and exam methods, he said. Also, one cohort was prospective while the other was retrospective, and slightly different reference standards were used to define true positivity.
"Nonetheless ... C-RADS was able to track the expected cohort differences, in particularly a larger number of E3s, E4s, and C4s at MGH, and C-RAD was also useful in analyzing practice patterns," Zalis concluded. "C0 results were used to modify practice and referral patterns."
By Eric Barnes
AuntMinnie.com staff writer
January 9, 2006
Related Reading
Low incidence of serious extracolonic findings seen in VC screening population, December 18, 2006
Advanced electronic cleansing preserves soft tissues in VC, October 11, 2006
VC gets long-awaited reporting standards, November 2, 2005
Copyright © 2007 AuntMinnie.com