Virtual colonoscopy practitioners have a new and potentially useful way to identify colorectal polyps at increased risk of harboring high-grade dysplasia or cancer, a study from the National Institutes of Health (NIH) suggests.
It is established in the literature (though less well known by radiologists) that barium-based oral contrast adheres to the surface of colorectal polyps. Studies demonstrating this adherence were completed years ago in an effort to develop better contrast agents.
It now appears that barium contrast is especially adherent to tubular adenomas and those with villous histology. And because barium contrast is routinely given to VC patients to help tag residual stool -- its presence could potentially alert radiologists to the need for further evaluation of higher-attenuating contrast-coated polyps at VC.
Villous histology in adenomatous polyps is a well-known indicator of increased risk of malignancy, said Dr. Ronald Summers, Ph.D., from the NIH in Bethesda, MD.
"Ninety-five percent of colorectal cancers arise from adenomatous polyps, but only 5% of adenomas progress to cancer," he said in a presentation at the 2005 International Symposium on Virtual Colonoscopy in Boston. "Villous histology is a risk factor for progression. Most adenomas don't have a villous component, but of cancers, a majority have a villous component."
The study led by Stacy O'Connor, along with Summers, Dr. J. Richard Choi, and Dr. Perry Pickhardt, was subsequently published in the Journal of Computer Assisted Tomography (January/February 2006, Vol. 30:1, pp. 51-57).
The group retrospectively examined CT data from 216 patients (147 men and 69 women, mean age 59.2) with polyps 1 cm or larger. The researchers borrowed their VC cases from the multicenter trial data published in 2003 by Pickhardt et al from the U.S. Department of Defense (New England Journal of Medicine, December 4, 2003, Vol. 349:23, pp. 2191-2200).
All subjects underwent cathartic cleansing with a sodium phosphate prep and 10 mg of bisacodyl 24 hours before VC and same-day optical colonoscopy. Along with a clear liquid diet, patients consumed 500 mL of barium sulfate (2.1% by weight, Scan C, Lafayette Pharmaceuticals, Lafayette, IN) for stool tagging, and 120 mL of diatrozoate meglumine and diatrizoate sodium (Gastrografin, Bracco, Milan, Italy) in divided doses.
Colonic insufflation was achieved manually with room air, self-administered by patients to maximum tolerance. All were imaged on a four- or eight-detector MDCT scanner (LightSpeed or LightSpeed Ultra, GE Healthcare, Chalfont St. Giles, U.K.). Collimation was set at 2.5 mm or 1.25 mm, respectively, with 1-mm overlapping reconstruction, 100 mAs, and 120 kVp.
Subjects in the NIH study cohort had one to eight colonoscopically proven polyps per patient, Summers said. In all there were 338 polyps in total; 207 were adenomas, 29 with a villous component (villous or tubulovillous histology), two cancers (both with a significant villous component), and 129 nonadenomatous polyps, including hyperplastic polyps, lipomas, etc.
On supine and prone imaging, 338 polyps were identified on 611 of the scans, Summers said. By consensus of two reviewers, lesions were divided into three categories with regard to contrast adhesion status, including:
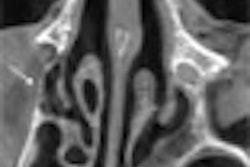
- Lesions with a thin adherent layer of contrast material, less than 2-mm thick ("You can see it as a thin layer of white etching on the surface of the polyp," Summers said.)
- Lesions without adherent contrast
- Lesions (surrounded by a pool of contrast material), which were excluded from further analysis
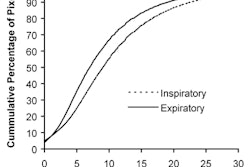
After excluding group 3 lesions surrounded by contrast, the results were evaluable for 312 of the 338 polyps. In all, 46% (144 of 312) had adherent contrast. Of the polyps with villous histology, 77% (20 of 26) had adherent contrast, for a sensitivity of 77%.
"Of the nonvillous polyps, 124 of 286, or 43%, had adherent contrast, so you can see the difference: 77% versus 43% (specificity 57%), which was statistically significant at the (p < 0.001) level," Summers said.
An odds ratio used to assess the odds of villous histology combined with an absence of adherent contrast showed that polyps with villous histology were significantly likelier to have adherent contrast than those without (p < 0.001). That is, for polyps with villous histology and without, the positive and negative likelihood ratios of having adherent contrast or not were 1.77 and 0.41, respectively. Conversely, the odds ratio for villous histology for polyps with adherent contrast compared to those without was 4.4% (95% CI, 1.7-11.2).
Lesions without a villous component could also be coated. The rate of contrast adherence for tubular adenomas was 44% and 43% for hyperplastic polyps. And not surprisingly, polyps with a villous component were significantly larger than those without (average 14.7 mm and 7.4 mm [p <0.001]).
"As you are aware, villous histology increases significantly in frequency as polyps get larger, so we needed to tease out the influence of polyp size on this observed finding," Summers said. For this task, multiple logistic regression analysis was used to account for factors such as polyp size, the presence of adherent contrast, or interaction of the two. The results showed a marked increase in the probability of villous histology with increasing polyp size when the polyp had adherent contrast.
Shape was also significant: 24% of flat lesions, 68% of pedunculated lesions, and 45% of sessile lesions (p = 0.0005) had adherent contrast.
"What we found was that size and (shape) ... were both statistically significant factors determining whether there would be adherent contrast or not," Summers said. As expected, for polyps over 10 mm, the odds of having villous histology increased tremendously, while the effect in medium-sized polyps (6-9 mm) was more subtle.
Why does contrast adhere to certain lesions? "We have two hypotheses that we're currently in the process of working on and figuring out which is the cause," he said. "The first hypothesis is that contrast adheres to the polyp due to its villous architecture; the oral contrast insinuates itself into the crypts in the villous arch, and hence appears as a thin adherent layer. Our second hypothesis is that contrast adheres to abnormal mucus made by villous polyps. It's a known fact that villous polyps produce mucus which is abnormal."
For now, radiologists examining VC patients should be aware that oral contrast agents often tag polyp surfaces in a pattern that is clearly distinct from internal tagging of adherent stool, and the differences must be recognized during interpretation, he said. And CAD systems will need to be able to avoid confusing coated lesions with tagged stool.
Larger studies are needed to confirm the significance of the findings, Summers cautioned. But if contrast-coated lesions are indeed higher-risk polyps, patient management could be altered as a result, particularly for those with medium-sized polyps (6-9 mm) for which surveillance is often recommended. (There were only five 6-9 mm polyps with villous histology in the cohort.)
"If it is verified that adherent oral contrast identifies polyps at risk for villous histology in the 6-9 mm category, including this criterion when determining the clinical significance of a polyp may lead to more appropriate recommendations for follow-up after (VC)," the group wrote in its published paper. "A polyp at risk for villous histology within this size category may merit a recommendation for immediate optical colonoscopy instead of short-term surveillance."
Research into contrast adherence might also lead to the development of more selective contrast media designed to hone in on riskier lesions, they added.
By Eric Barnes
AuntMinnie.com staff writer
March 15, 2006
Related Reading
Radiologists eye VC practice post-ACRIN, February 10, 2006
Adverse events weigh on colonoscopy mortality equation, February 6, 2006
VC fluid tagging optimized with barium on day of exam, January 23, 2006
Best preps are tailored to VC reading method, November 16, 2005
Copyright © 2006 AuntMinnie.com