The future is now for musculoskeletal ultrasound, owing to its cost-effectiveness for diagnosis as well as guidance of interventional procedures. But radiologists are losing control of the modality, according to research from Thomas Jefferson University (TJU) Hospital in Philadelphia.
Seeking to determine musculoskeletal ultrasound utilization trends, TJU researchers recently updated their 2002 research analyzing the technology's usage in the Medicare population. The study group examined the Health Care Financing Administration (HCFA) physician/supplier summary master files from 1996 to 2006, which include all Medicare Part B procedures.
The database covers 37.3 million fee-for-service Medicare beneficiaries as of 2006 and includes categories according to procedure codes, physician specialty, and place of service, according to Dr. Levon Nazarian, professor and vice chairman of education in TJU's department of radiology. He spoke during a session at the 2008 RSNA meeting in Chicago.
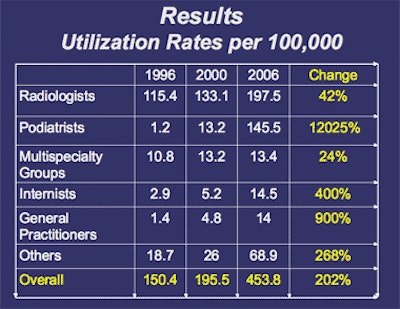
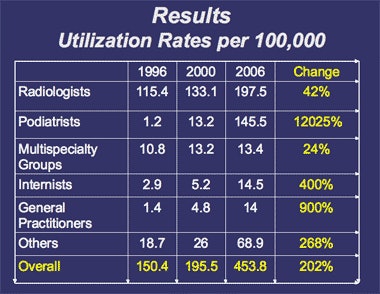
The researchers calculated utilization rates per 100,000 Medicare beneficiaries per year for studies with Current Procedural Terminology (CPT) 4 code 76880 (diagnostic ultrasound, extremity, nonvascular). Figures were calculated overall and by each physician specialty. The study team also calculated the rates of increase from the 1996 baseline to 2006.
 |
| Image courtesy of Dr. Levon Nazarian. |
Despite a 200% increase in musculoskeletal ultrasound studies during the decade, radiologist-performed exams only grew 42%, Nazarian said. The percentage of musculoskeletal ultrasound studies performed by radiologists also dropped significantly from 2000 to 2006.
Musculoskeletal ultrasound utilization by specialty
|
"We are now in the process of losing this modality in radiology because we're now under 50%," he said.
Other musculoskeletal ultrasound growth areas from the 2006 data included rheumatologists (2.6%), family practice - sports medicine (3.3%), orthopedic surgeons (1.2%), and physical med/rehab (1.1%), according to Nazarian.
Nazarian acknowledged several limitations of the study, including its use of Medicare data only and the inability to subdivide the data into the exact body part. Also, it wasn't possible to determine what specialty performs musculoskeletal ultrasound within multispecialty groups, he said.
Losing the turf battle
Radiologists don't utilize more musculoskeletal ultrasound for a variety of reasons, Nazarian said. They may consider it too operator- and equipment-dependent or be concerned about the technology's learning curve.
"Sonographers may be insecure with anatomy and pathology, and musculoskeletal radiologists may be insecure with ultrasound," he said. "And you often hear that it takes too much physician time, and, of course, time is money."
In addition, MRI is already well established, has a larger field-of-view, is better understood by referring clinicians, and perhaps most importantly, reimburses more, Nazarian said.
"If ultrasound paid better than MRI, we wouldn't be having this discussion," he said.
In response, Nazarian points out that MRI is also operator-dependent, given the expertise required to read those studies. In addition, the American College of Radiology (ACR) currently defines CT, CT angiography, MRI, MR angiography, PET, PET/CT, and radiation therapy as "complex procedures," which the organization fights hard to protect, Nazarian said.
"That must mean that either ultrasound is 'simpler' than MRI or that it's not worth fighting for," Nazarian said. "It's really one of those two; otherwise, why wouldn't the ACR list it as a complex procedure?"
Risks of ignoring musculoskeletal ultrasound
If radiologists don't perform musculoskeletal ultrasound, others will, Nazarian said. "Remember high-risk obstetrical ultrasound and echocardiography?" he said. "Both started in radiology."
And by radiologists dragging their feet, both ultrasound and MRI referrals may be lost. In addition, both diagnostic and therapeutic procedures are at risk, he said.
Even if radiologists wanted to win this turf battle, it wouldn't be easy for them. Most musculoskeletal radiologists are not truly subspecialty based; they are a cross between the modality and the organ system, Nazarian said.
In addition, most musculoskeletal radiologists don't even have ultrasound on their radar screens, he said. There also has been a lack of support by the ACR, he said.
For example, the ACR declined to support a new CPT code for shoulder ultrasound in 2005, both on initial application and appeal, Nazarian said. In explaining its decision, the ACR cited reasons such as obtaining only an estimated 15% increase in relative value units (RVUs) versus the 76880 CPT code, fear that in-code budget neutrality would decrease payment for 76880, and fear of shift of RVUs to other subspecialties, he said.
However, Nazarian said that musculoskeletal ultrasound should be done by radiologists. "We have the ultrasound training and expertise, we are better suited to perform correlative imaging when necessary, and there is less chance for self-referral," he said. "In any healthcare system, you want to control overutilization and reduce costs due to self-referral."
Advantages for nonradiologists
There are also arguments to be made for nonradiologists performing musculoskeletal ultrasound, including patient convenience. Patients can receive clinical evaluation and imaging in one visit, and ultrasound can serve as an extension of the physical exam, Nazarian said.
It could reduce costly MRI studies, provide guidance for interventions, and offer portability advantages, according to Nazarian. "It can bring ultrasound to athletic fields and other points of service," he said.
In addition, most radiologists are not interested in musculoskeletal ultrasound, and its potential is best appreciated by clinical physicians, Nazarian said. Also, they have a better appreciation of disease states and functional anatomy.
"They know the clinical history and differential diagnosis; radiologists may not know what they're looking for," he said. "And ultimately, the clinical physician has to face the patient and make them get better and make the proper diagnosis. If they think that ultrasound is the best and radiologists don't want to do it, they're going to find a way to provide that service."
One compromise would be for clinicians to have musculoskeletal ultrasound capability in their offices, scanning and reading the majority of cases themselves. If they can't answer the question, the clinician would then refer the patient to the radiologist, who can offer more experience and higher-end equipment, Nazarian said.
The American Institute of Ultrasound in Medicine (AIUM) held a practice forum in November, which led to the creation of short-term goals to develop performance and training guidelines for musculoskeletal ultrasound. In the long term, the organization hopes to tackle quality control and practice accreditation, according to Nazarian.
"The ultimate focus needs to be on the patient, who deserves to have musculoskeletal ultrasound competently performed, no matter who is performing it," he said.
By Erik L. Ridley
AuntMinnie.com staff writer
January 20, 2009
Related Reading
Ultrasound can boost imaging use in developing countries, November 21, 2008
Pictorial essay: 3D ultrasound reveals shoulder pathology, March 21, 2008
Ultrasound performs well in meniscal tears, February 5, 2008
Comprehensive musculoskeletal US exam offers most value, January 3, 2008
PACS offers direct access to MSK specialists without alienating rads, October 18, 2007
Copyright © 2009 AuntMinnie.com



















