Obese men with prostate cancer who receive external beam radiation therapy (EBRT) have a higher rate of biochemical failure and recurrence of cancer than their thinner peers. One reason for this, authors of a recently published study suggest, is that the delivered radiation dose may be off target.
The study evaluating prostate shift measurements of thin, normal, overweight, and obese men categorized by weight and body mass index (BMI) reveals that moderately to significantly obese men tend to have large shifts in prostate position in the left-right direction, and may receive a radiation underdose of as much as 30%, leading to treatment failure.
These findings, and the recommended solution of using image-guided radiation therapy (IGRT), were published in a recent issue of the International Journal of Radiation Oncology, Biology, Physics (December 2008, Vol. 72:5, pp. 1396-1401).
The department of radiation oncology at the Carol G. Simon Cancer Center of Morristown Memorial Hospital in New Jersey was the first cancer center in the U.S. to use image-guided radiation therapy for cancer treatments. In 2000, it installed a CT scanner on rails in a Primatom linear accelerator treatment suite, which incorporates a Somatom CT scanner on rails and a Primus linear accelerator (Siemens Healthcare, Malvern, PA). The suite was used for the localization of patient position during radiation delivery for prostate, lung, and liver cancer patients.
In 2005, when the cancer center replaced its existing equipment, it also replaced its treatment table with one designed to support patients weighing up to 550 lb, and acquired large-bore CT scanners (Somatom Sensation Open, Siemens) to accommodate very large and overweight patients.
The experience of Dr. James Wong, chairman of the radiation oncology department, and colleagues in measuring daily prostate shifts led them to hypothesize that patient obesity could have a direct impact on prostate shift during the course of receiving EBRT. These shifts, in addition to setup uncertainties in very obese patients, could lead to EBRT uncertainties, and ultimately to increased failure rate. They decided to measure prostate shifts in a selection of patients with thin to obese body types, and test the hypothesis that the amount of fatty tissue in the pelvic region was correlated with the extent of the prostate shift.
The researchers conducted a retrospective analysis using data for 117 consecutive patients who received IGRT between January 2005 and April 2007 at the Simon Cancer Center. Based on the National Institutes of Health body weight standards, 26.5% men were thin or of normal weight, 48.7% were overweight, 17.9% were mildly obese, and 6.9% were moderately to severely obese.
A total of 1,465 pretreatment CT scans obtained during 10 IGRT fractions for 58 patients and 15 fractions for 59 patients were analyzed, and the corresponding shifts in the daily movement of the prostate gland in the anterior-posterior (AP), left-right (LR), and superior-inferior (SI) directions were noted for each. Standard deviations of the target displacement from their planned position for each patient group (normal, overweight, mildly obese, and moderately to severely obese) were calculated.
The comparison of daily prostate displacement for the four groups revealed that patients with BMI values of 35 or greater, who are moderately to severely obese, tend to have large shifts in prostate position in the left-right direction as compared with patients in the other three groups.
Summary of prostate gland shift data during course of treatment
|
With increasing "subcutaneous adipose-tissue thickness," the distance measured at the isocenter from the skin to the underlying muscle of bone, a higher chance of skin shifting from side to side is possible, and thus an uncertainty of the actual amount of radiation delivered from fraction to fraction with conventional EBRT. When a patient is lying flat on a treatment couch, the anterior and left-right skin marks of the patient may not remain stationary relative to the alignment lasers in the treatment room.
IGRT, however, allows for the correction of target displacement at an extra cost, extra radiation dose of a daily CT, and extra time for each treatment procedure. The researchers did not calculate biochemical failure or cancer recurrence in this study because the patients had been treated too recently to have a meaningful long-term outcome.
Wong does not rule out the hypothesis that obese men may have more biologically aggressive cancer. But he told AuntMinnie.com that it would be interesting to see the same type of analysis conducted for prostate cancer patients who received IGRT as was performed for patients who received EBRT at the University of Texas M. D. Anderson Cancer Center in Houston. This study, with epidemiologist Sara Strom, Ph.D., as lead author, was published in Cancer (August 1, 2006, Vol. 107:3, pp. 631-639).
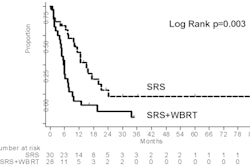
Strom and colleagues retrospectively analyzed the outcomes of 873 consecutive patients who exclusively received EBRT for localized prostate cancer between 1988 and 2001. The proportion of body weights of this large patient cohort was quite similar to the Simon Cancer Center's patients: 27% normal, 50% overweight, 18% mildly obese, and 5% moderate to severely obese. Of the total group, 34% had biochemical failure and 15% had a recurrence of cancer.
The researchers reported that men in the most obese group had a 99% greater risk of developing biochemical failure compared with normal-weight men. Obese men also had a significantly higher rate of clinical failure and a twofold risk of developing metastases compared with nonobese men after adjusting for all clinical and tumor characteristics and treatment factors.
The researchers also examined the potential for differences in radiation technique in obese and nonobese men. They noted that the patient cohort had received treatment at a time when a more simple conventional radiation technique was used, and alluded to the potential for setup error. Because margins were large enough to account for setup errors as great as 11.4 mm in the left-right side, the authors stated that it appeared unlikely that radiation technique alone could explain their findings.
Wong isn't quite convinced. He told AuntMinnie.com that the some of the moderately to severely obese patients in the M. D. Anderson study may have been underdosed. Citing an example of a 450-lb patient with a BMI of 45 and a subcutaneous adipose-tissue thickness of 17.8 cm, based on daily pretreatment CT scans for setup verification, the magnitude of setup error in 13 of 40 fractions was found to be more than 10 mm in the left-right direction. Had this patient been treated with a conventional 3D conformal technique, with a uniform margin of 10 mm, the patient might have been underdosed up to 30%.
By Cynthia E. Keen
AuntMinnie.com staff writer
March 23, 2009
Related Reading
Increasing BMI may impact choice of prostate cancer treatment, September 25, 2008
Obesity, overweight associated with increased prostate cancer mortality, November 19, 2007
Copyright © 2009 AuntMinnie.com