The good news is that U.S. hospitalization rates for cervical cancer declined by 36% in 2004, with the number of admissions falling from 34,600 to 24,800 in a 10-year period, according to the Agency for Healthcare Research and Quality (AHRQ).
The bad news is that more than 10,000 new cases of cervical cancer were diagnosed in 2005, despite the fact that screening for the disease is widespread and relatively simple, said the American Cancer Society. It remains to be seen if the generation of women who avail themselves of the new cervical cancer vaccine will see the disease all but disappear.
Several new studies took a closer look at the roles of imaging and radiotherapy for cervical cancer staging and treatment. In the first paper, researchers from Canada sought to make a connection between interstitial fluid pressure (IFP) and MR-derived kinetic-modeling parameters. In the second, the investigators from the American College of Radiology Imaging Network/Gynecologic Oncology Group (ACRIN/GOG) trial 6651/183 compared CT to MRI for initial, presurgical clinical assessment of cervical cancer.
Finally, oncologists and radiotherapists in Italy looked at lymph node involvement in cancer patients who were treated with preoperative chemoradiation versus chemotherapy.
IFP and tumor angiogenesis
Elevated pressure in malignant solid tumors and the resulting abnormal tumor microvasculature can lead to high IFP. Unfortunately, increased IFP has been linked to shorter disease-free survival and recurrence. While dynamic contrast-enhanced MRI (DCE-MRI) has been used to successfully study tumor angiogenesis, can it offer valuable information about IFP?
"Given the relationship of both IFP and DCE-MRI to the tumor microvasculature, we hypothesized that DCE-MRI-derived parameters may be related to IFP in cervical cancer," wrote Dr. Masoom Haider and colleagues from the University of Toronto, Mount Sinai Hospital, and Princess Margaret Hospital, all based in Toronto. "Such a relationship could provide insight into in vivo tumor physiology and treatment response" (Journal of Magnetic Resonance Imaging, January 2007, Vol. 25:1, pp. 153-159).
For the study, the group specifically looked at the following MRI-derived parameters -- all relative to muscle:
- Initial area under the enhancement curve (IAUC60m)
- Vascular permeability (rktrans)
- Extracellular volume fraction (rve)
The researchers enrolled 32 women, the majority (21) of whom had squamous carcinoma. All were candidates for radiation therapy with or without concurrent cisplatin chemotherapy.
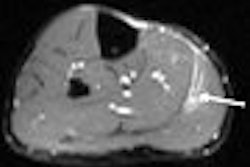
Imaging was done on a 1.5-tesla system with 0.1 mmol/kg of gadodiamide (Excite or EchoSpeed, GE Healthcare; Omniscan, GE Healthcare Bio-Sciences, Chalfont St. Giles, U.K) before treatment began. The IFP was measured in vivo after MRI and again before treatment. Cervical tumor was defined by the enhancement pattern and T2-weighted imaging. The mean tumor diameter as measured by MRI was 4.5 cm.
The results were as follows:
- Median IFP was 16.3 mmHg
- Median IAUC60m was 4.0
- Median rktran was 4.65
- Median rve was 2.56
The authors found no significant correlation between IFP and rve, and no correlation between tumor size on MRI and any of the DCE-MRI parameters. They did find a significant negative correlation between IAUC60m and IFP, and a moderate negative correlation between rktrans, IAUC60m, and IFP.
"It seems counterintuitive that IFP appears negatively correlated with permeability.... Perhaps the most likely explanation is that rktrans is not reflecting permeability alone but a combination of microvasculature features depending on permeability, capillary surface area, and blood flow," the authors wrote.
Still, this moderate negative correlation may still make DCE-MRI parameters valuable in assessing tumor behavior, they stated, adding that the IAUC60m measurement in particular is easy to perform and relatively insensitive to noise.
MRI for sizing up cervical tumors
In 2005, the ACRIN/GOG 6651/183 investigators released their preliminary results on the value of CT and MRI findings for the pretreatment evaluation of early invasive cervical cancer. They found that CT and MRI performed similarly, influencing the accuracy of International Federation of Gynecology and Obstetrics (FIGO) clinical staging (Journal of Clinical Oncology, December 20, 2005, Vol. 23:36, pp. 9329-9337).
However, at the 2005 RSNA meeting in Chicago, Dr. Hedvig Hricak gave MRI a boost over CT, stating that it was "significantly better than CT for tumor visualization (and) for detection of parametrial extension."
The primary end point of the ACRIN/GOG 6651/183 study was the role of imaging for staging. In a secondary analysis, the group, led by Dr. Donald Mitchell, looked at the additional end point of tumor delineation.
The patient population consisted of 172 women with biopsy-confirmed cervical cancer who had agreed to CT and MRI studies. The majority of the women were diagnosed with squamous cell carcinoma (72%) and were FIGO stage IB (65%). All tumors were less than 5 cm in diameter.
The minimum standards for contrast-enhanced CT imaging were spiral data acquisition at 5-mm collimation during suspended respiration. The minimum standards for noncontrast-enhanced pelvic MR included:
- 1.5-tesla field strength
- Phased-array surface coils
- Axial and sagittal fast spin-echo T2-weighted images of the pelvis
- T1-weighted axial images from pubis to renal hila
All images were read and graded on a five-point scale (1 = cancer definitely absent; 5 = cancer definitely absent) for the likelihood of cervical stroma and uterine body involvement. Each study was interpreted prospectively by one radiologist, then retrospectively by four other readers.
According to the authors, neither MR nor CT was accurate for evaluating cervical stroma and uterine body involvement. But based on the ROC curve analysis, MR produced a higher AUC than CT for the primary reader (0.80 for MRI and 0.66 for CT; p = 0.01) and for retrospective readers (0.68 for MRI and 0.57 for CT; p = 0.02).
Among the CT primary readers, 38% rated cervical stromal invasion as indeterminate versus 5% of the MRI primary readers. The retrospective readers could measure tumor diameter on CT in 35% to 73% of the patients. These same readers measured diameter on MRI in 79% to 94% of the patients.
"Our results ... showed higher agreement and correlation with pathology for MRI than for CT or clinical assessment.... Not only was CT less accurate, but CT readers could not even record measurements in most instances," the authors wrote. "If an expert reader cannot measure a tumor, delineating its margins for treatment planning is likely to be problematic" (Journal of Clinical Oncology, December 20, 2006, Vol. 24:36, pp. 5687-5694).
The group acknowledged that developments in multislice CT may help the modality overcome its shortcomings (poor soft-tissue contrast, low correlation with pathology) for measuring cervical tumors. But CT exams would still require a contrast agent and, of course, pose a radiation risk.
On the other hand, "MRI can be used to delineate gross tumor margins without contrast enhancement in most patients, as shown in this series," the authors noted. "Current MRI technology seems well-suited for delineating tumor boundaries."
Lymph node involvement
A big issue in cervical cancer management is the control of lymph node disease, according to Dr. Gabriella Ferrandina and colleagues from University of Rome and the Catholic University of Campobasso, both in Rome.
"Concurrent chemoradiation has been widely recognized as the golden standard for the management of bulky stage IB and locally advanced cervical cancer," Ferrandina's group wrote. "The availability of preoperative and/or intraoperative predictors of lymph node involvement would be of utmost clinical relevance in order to individualize treatment" (Annals of Surgical Oncology, January 7, 2007).
The researchers hypothesized that control of pelvic disease achieved with comitant chemoradiation, versus neoadjuvant chemotherapy (NACT), might positively alter the rates and patterns of lymph node involvement.
The study included 127 patients. Based on MRI scans, the women were diagnosed with squamous cell carcinoma with no evidence of para-aortic node involvement. They were then given chemoradiation or NACT before radical surgery.
Radiotherapy was administered to the whole pelvic region in 22 fractions (1.8 Gy/day for a total of 39.6 Gy) in combination with cisplatin. Cisplatin-based chemotherapy also was done for two to three cycles.
The authors explained that patients who responded completely or partially to treatment then went on to surgery. Patients with no change or disease progression were candidates for salvage chemotherapy.
Overall, the group found that the percentage of cases with metastatic lymph node involvement was significantly lower when chemoradiation was administered (11.5%) versus NACT (30%).
In terms of the pathologic response, microscopic tumor response was recorded in 75.9% of the cases that underwent chemoradiation, compared with 22.5% of the cases that had NACT. But NACT bested chemoradiation NACT for macroscopic response with partial response or stable disease -- 77.5% versus 24.1%.
"The overall number of removed para-aortic lymph nodes did not differ according to (the) type of neoadjuvant treatment ... and there was no difference in the rate of metastatic involvement at para-aortic level," the authors noted.
However, the number of lymph nodes detected in the parametrium was significantly lower in chemoradiation cases (median three) versus NACT cases (median five; p = 0.002).
"Chemoradiation seems to lessen more than 60% the chances of finding cases with positive pelvic lymph nodes compared to patients administered NACT.... In (the chemoradiation)-treated group, MRI-assessed pelvic status after treatment correlated with pathological findings," the group concluded.
In addition, there is the possibility that the pathological status of the lower pelvic nodes could be predictive of the pathology of lymphatic diffusion in cervical cancer. The next phase of research in this area will have to focus on how the high rate of pelvic control achieved with chemoradiation affects disease recurrence and clinical outcome, the authors stated.
By Shalmali Pal
AuntMinnie.com staff writer
January 23, 2007
Related Reading
MR makes clinical, technical strides in imaging the female pelvis, November 17, 2006
PET/CT shows strength for staging cervical cancer, May 31, 2006
Smoking increases risk of squamous cell cervical cancer, April 17, 2006
MRI ready for prime time in cervical cancer diagnosis, November 27, 2005
Copyright © 2007 AuntMinnie.com