Electronic medical record (EMR) systems allow alerts regarding critical results of abnormal imaging exams to be transmitted at record speed to referring physicians. But this doesn't mean that the recipients are reading these important findings, according to a new study released in the Archives of Internal Medicine.
Researchers studied response to an automated critical results notification system at the Michael E. DeBakey Veterans Affairs Medical Center (VAMC) in Houston and its five affiliated outpatient clinics over a six-month period. They found that while the vast majority of alerts regarding abnormal imaging findings were heeded, 7.7% of alerts were ignored. Nearly all of these alerts had a measurable clinical impact on patients, including 11 cases of cancer (Arch Intern Med, 2009, Vol. 169:17, pp. 1578-1586).
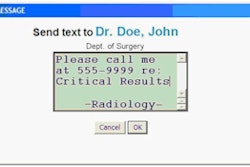
The EMR used by all VAMCs relies on a notification system -- a "View Alert" window -- to alert clinicians about critical test results of radiology exams. Clinicians depend upon the View Alert system for abnormal test results, because it's the only way that they receive notifications about exam and laboratory reports ordered for their patients. The exception is when physicians are personally telephoned by radiologists about life-threatening findings.
All diagnostic tests and examinations at the VA are ordered through a computerized order entry system, and results are electronically conveyed to a patient's medical record. Whenever a medical professional opens a patient's record, the event is tracked.
Alerts transmitted to physicians by the critical findings notification system are electronically monitored, noting the time and individual(s) who open them. When an imaging procedure is ordered by a physician other than the primary care provider, both doctors receive the alert of abnormal findings. Physicians who will be off-duty or on vacation can transfer alert notifications to a designated backup physician.
Alerts remain posted in the View Alert window, dropping off the queue when opened and after two weeks if unopened. Because radiology reports of abnormal findings are added to patients' medical records, it is possible for a clinician to read the report findings without opening the corresponding alert notification in the View Alert window.
What happened
From November 2007 through May 2009, a total of 123,638 outpatient diagnostic imaging exams were performed, with accompanying radiology reports. Critical-finding alerts were generated for 1,196 exams, or 0.97% of the total. Radiologists personally notified physicians of 206 of these alerts (17.2% of alert total). The EMR recorded that 81.9% of the alerts were acknowledged by their recipients.
The study showed that 217 alerts were not opened for up to 28 days after being posted, and no evidence of documented follow-up action was recorded for 131 of them. Of these, the study authors identified 111 cases that merited timely follow-up.
The researchers telephoned each recipient of an unopened critical event alert to find out if undocumented follow-up had occurred and if any intentional decision had been made not to follow up, according to principal investigator Dr. Hardeep Singh, co-director of the Houston VA Center of Inquiry to Improve Outpatient Safety through Effective Electronic Communication. Singh and colleagues downloaded data on a weekly basis and, therefore, were able to contact physicians during the fifth week of inactivity for every alert.
Ultimately, 92 alerts were identified as lacking timely follow-up four weeks after posting. After the research team made its call to a physician, 50% of the cases were followed up within seven days after the call.
How important were these 92 alerts?
Twenty-six alerts, or 28%, represented new diagnoses of disease for 26 unique patients, of which 11 were diagnoses of cancer. In addition, 100 additional diagnostic imaging procedures and seven laboratory tests were ordered for 64 patients, of which 57% identified abnormal findings in 41 patients. Seventeen invasive diagnostic tests were performed for 16 patients, 64.7% of which had abnormal findings for 10 patients.
Twenty patients required treatment with hospitalization, and six of these patients had surgical procedures. Two patients died of symptoms or disease identified as the primary diagnosis of the radiology procedure.
The most ignored type of abnormal findings alerted clinicians to chest imaging showing a nonspecific density. Sixty-two of the 92 alerts were related to some form of suspected new malignant neoplasm. If the authors had not intervened, all had the potential to lead to missed or delayed diagnosis.
Dual-alert notification, designed as a safeguard and to protect against lack of follow-up, proved to be just the opposite. The researchers found that sending alerts to two physicians rather than just one actually increased the likelihood that an alert would be ignored: 53 of the 92 exam alerts were sent to at least two physicians and were ignored by both.
"Preliminary evidence from our study suggests that [healthcare providers] may believe responsibility for follow-up belonged to someone else," Singh and colleagues said.
Recommendations
The authors recommended that the next generation of electronic medical records create better tracking and automated reminder systems and incorporate care coordination programs. Until such systems become available, they suggest the following:
- Policies should be developed and publicized with respect to who is responsible for responding to a critical results alert and the time frame to respond.
- Unacknowledged alerts must stay active in View Alert windows for longer periods of time than 14 days, and should perhaps stay active indefinitely.
- Alerts posted in the View Alert queue should require the signature of the ordering healthcare provider and a statement of action before they are removed from the queue.
- The existing EMR should be automated to track not just acknowledgement but the specific response documenting that appropriate action has been taken for each abnormal alert.
- Audits and performance feedback systems should be established to give hospital or healthcare enterprise administrators and healthcare providers information on timely follow-up of patients' test results on a regular basis.
By Cynthia E. Keen
AuntMinnie.com staff writer
September 28, 2009
Related Reading
Automated emails reinforce radiology reports for important findings, August 26, 2009
Critical results reporting -- it's cheaper than settling lawsuits, June 5, 2009
New search tool finds the needle in PACS haystack, May 1, 2009
Communicating abnormal findings may not ensure follow-up, November 28, 2007
Copyright © 2009 AuntMinnie.com