BERLIN - It's like the weather. Radiologists complain that their CAD software isn't integrated well enough with their PACS networks, but they never do anything about it.
Until now, they really couldn't. If you wanted to view CAD markings from your PACS workstation, you were largely limited to CAD software made available through OEM relationships inked by your PACS vendor. If they didn't have your preferred CAD solution, you were largely out of luck -- or were facing an expensive custom integration effort.
But after two and a half years of sweating the details, a team led by researchers from the University of Southern California in Los Angeles has developed a home-grown method for integrating CAD with PACS regardless of the vendor, bringing CAD into the sunlight of daily workflow.
With a little hard work, they say, CAD results from virtually any vendor can be stored on just about any PACS for permanent reference, manipulation, quantitation, research -- you name it. That's right, no more running back to the CAD workstation to recheck the results, or to calculate the average number of false-positive detections in symptomatic patients over a year's time.
To be sure, CAD and PACS developers have already taken steps to incorporate the use of some CAD packages on their networks. But the USC method is vendor-independent, and allows for multiple CAD products to be installed on the same PACS network, according to the researchers.
To incorporate it in your practice you'll need an experienced IT person with significant DICOM experience, however.
"Why do we need PACS-CAD integration?" Dr. H.K. (Bernie) Huang asked attendees on Thursday at the Computer Assisted Radiology and Surgery (CARS) meeting. "Mostly for imaging data, PACS infrastructure, and clinical integration.... I'll introduce a CAD-PACS toolkit that seamlessly integrates multiple CAD methods into your PACS clinical operations."
Going back to the CAD workstation every time you need to work with a patient's CAD results is time-consuming, and it interrupts workflow, said Huang, who is a professor of radiology and biomedical engineering at the University of Southern California and chair of medical informatics at the Hong Kong Polytechnic University in Kowloon, Hong Kong.
The PACS' DICOM reporting structure is ideal for tracking many CAD applications, he said. Take multiple sclerosis (MS), a progressive neurological disease that results in multiple white-matter lesions on MRI (T1 and FLAIR images).
Making a diagnosis on MRI is not difficult, but it is time-consuming to quantify the number and size of lesions, Huang said. Imaging informatics is the ideal quantitative tool to monitor progression of MS. And a DICOM-structured report image can be used to overlay lesions representing ground truth in one color, with CAD output and patient images over time in different colors. A separate report tracks each lesion, its size, and location, and when it was first visualized. The composite report image can be stored in 3D on a PACS server, available for viewing, manipulation, and research.
To enable PACS-CAD integration, the group has devised two versions of what it calls the CAD-PACS toolkit. First and easiest to implement is a version called the DICOM-SC (secondary capture) toolkit, Huang said. The second and more functional version is called the DICOM-IHE (Integrating the Healthcare Enterprise) model.
"Let's take a look at the typical CAD workflow," Huang said. "You have a modality, you have the RIS, and both methods you can use to push the images from CAD to the diagnostic workstation. And from there the (technologist) or radiologist can send the data to the CAD workstation. Ninety-nine percent of the time the vendor or researcher who developed the CAD method kept the results on the CAD workstation. You very seldom can push the information to the PACS server and workstation, and this tool can allow you to do just that."
Step-by-step DICOM-SC (version 1)
In the easier DICOM-SC implementation of the toolkit, which the team calls i-CAD-SC, the tool creates a screen shot from any CAD application output, Huang said. An i-CAD convert function exists to convert the CAD output screen shot into a DICOM file. Another component called DICOM C-Store SCU automatically sends the DICOM file to the PACS for storage, he said.
DICOM-SC workflow begins with the PACS workstation sending DICOM files to the CAD workstation for processing. "The CAD workstation receives the DICOM files and then performs the processing," Huang said. The DICOM-SC with the i-CAD-SC package installed on the CAD workstation then converts the screen shot of the CAD results to DICOM files, and sends it to the PACS server, which stores it as an additional series labeled as the CAD results under the same patient study that already exists in the PACS server.
"When the PACS workstation queries the PACS server, the new series containing the CAD results will appear as a series under the (existing) study of the patient," Huang said. The physician can then retrieve the CAD results with the study to his or her PACS workstation as a DICOM image. This is the simplest method, and you can retrieve this data anytime you need it, he said.
On the down side, "you see what you get," Huang said. "You cannot take the data from the screen shot and use it for future analysis and data mining purposes." That is, the output is static and cannot be manipulated for broader research purposes, he explained. The way to do that is more complicated, and involves installing a separate server on the PACS to store the fully interoperable CAD output data.
Step-by-step DICOM-IHE
The DICOM-IHE version of the toolkit contains the following elements:
The i-CAD component creates DICOM-SR objects from CAD output, which are sent to the PACS. i-CAD also queries the CAD worklist in the i-PPM (postprocessing manager), a key component that enables CAD results to be transferred from the CAD workstation to the PACS for processing, Huang said. i-CAD also exchanges general-purpose scheduled procedure objects for scheduled work items.
i-PPM also provides the functionality needed to schedule and track the status of PACS-CAD workflow, he said. A Receive-SR component provides a database to store structured reporting results, and supports DICOM query/retrieve functions from the PACS workstation. Finally, the Display-SR module serves as a display Web server with DICOM-SR C-store and C-find functionality.
DICOM-IHE workflow goes like this: First the CAD workstation queries the CAD worklist from the i-PPM. The CAD lists the work items to be performed. The CAD workstation then retrieves the DICOM images from the PACS server for CAD processing.
Meanwhile, the CAD workstation sends out a "work item in progress" message to the i-PPM, and the PACS server pushes the DICOM worklist to the i-PPM requesting CAD processing of the studies, Huang said. The CAD workstation performs the processing, and stores the CAD results in the Receive-SR installed on the PACS server.
In return, the CAD workstation outputs work item PPS and work item completed messages to the i-PPM. Finally, the PACS workstation retrieves the DICOM-SR CAD results for the radiologist's review. The Web-based Display-SR component can be used in the PACS workstation to view the CAD results.
"That completes the data flow of PACS and CAD together," Huang said. It's not a project for IT beginners -- "you need a lot of understanding of DICOM," he said. But it does work.
Huang offered two examples of lung CAD output. The secondary capture image showed the original CAD output as a static image with an arrow on the lung lesion. The second image, representing the same lung CT image but in the DICOM-IHE version, provided a DICOM-structured report adjacent to the image.
"If you want to see a nodule, you just click on it," he explained. The process is ideal for training readers, and for building, storing, and querying large comparative databases such as the group's bone age assessment project for children.
The DICOM-IHE setup also shines for comparing and analyzing CAD output from multiple modalities, Huang said. For example in breast imaging there might be full-field digital mammography, contrast-enhanced MRI, and 3D ultrasound images of the same patient. If you're a physician at a women's clinic you can put all of them together for easy cross-referencing.
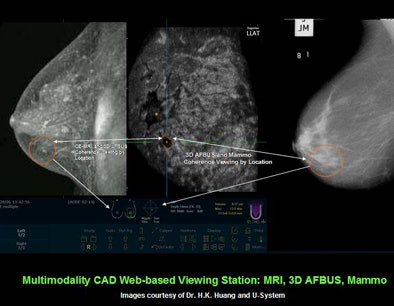 |
| Images courtesy of Dr. H.K. Huang and U-System. |
"That's the power of PACS-CAD integration" Huang said. "It's a one-stop shop. You can get clinical diagnosis, clinical services, decision support, and also training."
For both the simpler DICOM-SC version and DICOM-IHE toolkits, "our experimental integration of CAD applications to diagnosis workflow shows the efficiency of two methods to integrate independent CAD results with a PACS seamlessly," he said.
A paper describing the project, "CAD and Image-Guided Decision Support," has just been published by Huang, Kunio Doi, et al (Computerized Medical Imaging and Graphics, June-July 2007, Vol. 31:4-5, pp. 195-197).
By Eric Barnes
AuntMinnie.com staff writer
June 29, 2007
Related Reading
Fully automated VC CAD system solves tagging problems, June 25, 2007
Automated analysis tools vary in pulmonary nodule measurements, June 25, 2007
CAD performs well in lung nodule detection, February 5, 2007
Lung CT CAD boosts performance of less experienced radiologists, November 27, 2006
Colon CAD: VC's extra eyes face new challenges, August 5, 2005
Copyright © 2007 AuntMinnie.com