Like many other specialties, anesthesiologists are feeling the crunch of the medical manpower shortage. The situation can affect imaging directly when pediatric sedation is required for MRI exams. At the Texas Children's Hospital in Houston, anesthesiologists organized a sedation service for staffing the MR suites at their tertiary care pediatric center. They discussed their experience at the 2007 American Society for Anesthesiologists (ASA) meeting in San Francisco.
Meanwhile, two published papers also scrutinized pediatric sedation techniques for MR exams. A group in Italy sought to determine if children with a lysomal storage disease required specialized sedation, while anesthesiologists in Buffalo, NY, tested the feasibility of using a new, fast-acting sedative in magnet-bound children.
Sedation service
"In our anesthesiologist-directed sedation service for diagnostic imaging, we have credentialed nonanesthesiologists to use propofol," said Dr. Laura Torres during her ASA talk. "Our primary objective was patient safety. Our second objective was clinical productivity. To meet the demand for manpower, we recruited the help of our critical care medicine faculty colleagues."
Torres said the group chose critical care medicine physicians because they are skilled in handling hemodynamic instability, stressing that the group was under the constant supervision of anesthesiology and did not run an independent sedation service.
Another goal of the sedation service program was to minimize or even eliminate failed sedation cases, added Torres, who is also an assistant professor in pediatric anesthesiology at Houston's Baylor Medical College.
The sedation team consisted of 2.5 full-time employee (FTE) critical care medicine physicians and 25.8 FTE nurses. To qualify for the service, participants underwent training that included MRI safety guidelines.
Patients were sedated either by a physician or a nurse, depending on their health status. Sedation service nurses were authorized to administer chloral hydrate to infants and midazolam/pentobarbital to older children. The physicians administered propofol and were limited to a maximum dose of 175 mg·kg·min infusion rates. Anything higher than that dose required consultation with the anesthesiologist, Torres said.
For statistical analysis, patients were divided into group one (presedation service) and group two (postsedation service). According to the results, the average daily census of completed scans increased by 19.6% after sedation service was introduced. In addition, the backlog for routine studies decreased by 24.3%, with the most dramatic results in 30-minute, contrast-enhanced brain MR studies, Torres said.
|
The team also found fewer incidences of hypoxemia (down to six cases from 18) in group two because the sedation service team was able to intervene and rescue the airway, Torres said.
Finally, Torres and colleagues found that anecdotally, the nonanesthesiology professionals praised the service for bolstering a more cooperative relationship among specialists. An ancillary goal of this project was to coordinate sedation requirements with surgery, other interventional procedures, and/or other imaging studies, Torres said.
"In this study, we have shown that operational efficiency and patient safety improved in an anesthesiologist-led service model," the group wrote in its ASA abstract. "We have used this information to negotiate with the hospital (to receive) increased funding for our department of anesthesiology as we expand our service," Torres added. Hospital billing for MR-related sedation increased by 20% after the sedation service was implemented, according to the ASA poster.
In response to an ASA session attendee question, Torres explained that the increased funding did mean more hires for her department, but that didn't leave the sedation service team high and dry, as demand for imaging services has continued to grow. She noted that when the sedation service started, there were two 1.5-tesla MR scanners. Since then, the hospital has added two more scanners, which means four scanners that require staffing by the sedation service.
ASA session moderator Dr. Rita Agarwal asked why there were cases of failed sedation if this group was specifically trained to provide this service. Torres said failure occurred for three nurse-administered procedures and one physician-administered exam because of the sedation dosing limits placed on them.
MLD patients
Metachromatic leukodystrophy (MLD) involves the central and peripheral nervous systems (CNS and PNS), causing developmental delay, psychomotor regression, ataxia, and other neurological disorders, according to neurosurgical anesthesiologists Dr. Cristina Mattioli and Dr. Marco Gemma, and their colleagues from the Scientific Institute Hospital S. Raffaele in Milan. Neuroradiologist Dr. Cristina Baldoli also contributed to this research.
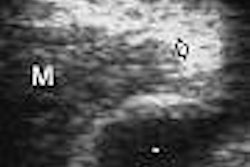
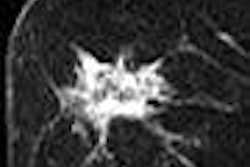
MLD before age 2 is considered late-infantile, while the juvenile form strikes children between ages 4 and 12, they said. "MRI has a fundamental role in the diagnosis of MLD. It shows diffuse white-matter signal alterations, such as characteristic hyperintensity in T2-weighted sequences and, quite frequently, a striated (tigroid) pattern. "The advanced stages of the disease can show focal or global cerebral atrophy" (Pediatric Anesthesia, January 2007, Vol. 17:1, pp. 64-69).
Unfortunately, the risk of an adverse event for MR-related sedation, such as aspiration or other respiratory impairment, in MLD children is not particularly well-known, they explained. For their study, the researchers enrolled 10 late-infantile patients who were sedated with thiopental (T_MLD). Eight juvenile patients were sedated with propofol (P_MLD). A control group consisted of 20 age- and sedative-matched children who underwent brain MRI for suspected seizures, but were not diagnosed with MLD (T_HLT and P_HLT).
Upon arrival in the neuroimaging suite, a warmed crystalloid infusion was administered intravenously to all subjects. Groups T_MLD and T_HLT received 5 mg·kg-1 thiopental, while groups P_MLD and P_HLT received 1.0-1.5 mg·kg-1 propofol.
Imaging was done on a 1.5-tesla scanner and possible complications were recorded including hypoxia, convulsions, and MRI artifact movements. The children were covered with blankets during the 30- to 45-minute scans. Fifteen minutes after the MR exam, children were evaluated by the anesthesiologist and were discharged only if their neurological status returned to pre-MRI levels.
According to the results, no complications occurred during sedation or recovery. The authors also found no significant difference in the mean doses of sedative to induce patient immobility in the MLD group or the control group:
- 0.227 ± 0.053 mg·kg-1·min-1 for T_MLD
- 0.119 ± 0.061 mg·kg-1·min-1 for T_HLT
- 0.119 ± 0.061 mg·kg-1·min-1 for P_MLD
- 0.115 ± 0.043 mg·kg-1·min-1 for T_HLT
"When evaluating a sedation strategy for radiology, it is crucial to assess its efficacy in maintaining patient immobility," Mattioli's team stated. "In all our MLD cases, MRI was completed and the image acquisition took place over a similar time span as with normal children undergoing MRI under sedation."
In an e-mail to AuntMinnie.com, Gemma stated that this sedation protocol is now used routinely in MLD children who are slated for an MR exam. Target-controlled, computer-driven propofol infusion has also shown promise to maintain patient immobility, he said.
Dexmedetomidine
The upside of the short-term intensive care unit sedation agent dexmedetomidine is that it has a rapid redistribution half-life of nine minutes and an elimination half-life of 110 minutes in children. In addition, it provides sedation with less risk of respiratory depression, although possible side effects include bradycardia and hypotension.
Anesthesiologist Dr. Christopher Heard and colleagues at State University of New York in Buffalo reviewed their initial clinical experience with dexmedetomidine in a series of case reports.
At their institution, the standard dexmedetomidine dose is a bolus of 0.5 mg·kg-1 and infusion of 1 mg·kg-1·h-1, Heard's group stated. For this retrospective review, 21 patients (mean age 3.3 years) underwent sedation for a one-day MRI procedure. The mean scan time was 62.7 ± 25.7 minutes, and the total dexmedetomidine dose was 1.79 ± 0.59 mg·kg-1.
According to the authors' research, five of the first eight patients moved in the scanner, which required the rescanning of one to three sequences per exam. All five patients were given supplemental sedation with propofol (dose range from 1.5-5.5 mg·kg-1) to good effect. After patient eight, a 0.1 mg·kg-1 bolus of midazolam was added to the sedation regimen, after which only one patient moved. However, this patient had an hour-long scan.
"In the initial eight patients, the movement occurred at an average time of 36 minutes. In all patients, the longer the scan time the more likely movement was," the authors wrote. "It was also noted by the anesthesiologist that when the patients moved there was very little warning that the depth of anesthesia was inadequate" (Pediatric Anesthesia, September 2007, Vol. 17:9, pp. 888-892).
Heard's group suggested that the standard cardiovascular parameters used to judge the depth of anesthesia are inadequate in this patient population. Other options for measuring the depth of anesthesia include electroencephalogram (EEG), EEG entropy, and spectral frequency index monitoring.
"It appears that we require deep sedation to facilitate the MRI scan," the group wrote. "Dexmedetomidine by itself proved to be unpredictable with respect to either adequate dosing or the duration of recovery."
In other pediatric sedation news, several presentations at the 2007 RSNA meeting in Chicago will take a closer look at this subject. In a focus session, Dr. Bernadette Koch and colleagues from the Cincinnati Children's Hospital Medical Center will review the current standard of care for pediatric sedation, including the Joint Commission's recommendations and requirements (SFN02).
Also, a group from Boston's Harvard University will discuss radiologist-administered ketamine sedation for children undergoing renal and kidney biopsies (LL-PD2074-H05). Another education exhibit will compare MRI versus CT (less sedation) for assessing the congenital causes of vascular airway narrowing (LL-VI5138).
By Shalmali Pal
AuntMinnie.com staff writer
October 25, 2007
Related Reading
Three-tesla cardiac MRI of preterm infants does not require sedation, July 19, 2007
Mock MRI exam preps children for the real deal, November 30, 2005
Hypnosis relieves distress of voiding cystourethrograms in children, January 5, 2005
Sleep deprivation does not improve pediatric sedation failure rates, May 31, 2004
Copyright © 2007 AuntMinnie.com