
Until an endorectal coil specifically designed for use with the 3-tesla MR system is readily available, prostate imaging at 1.5 tesla will continue to be preferable, according to a report in the American Journal of Roentgenology.
The introduction of endorectal surface coils has greatly improved the signal-to-noise (SNR) quality of prostate imaging at 1.5 tesla, but the accuracy for cancer staging is still in flux, ranging from 51% to 89%, explained Dr. Dirk Beyersdorff and colleagues from Charité Universitätsmedizin in Berlin. On the other hand, 3-tesla MR offers better SNR but no endorectal coil has been approved for use with these scanners, and phased-array torso coils have fallen short, they added.
Beyersdorff's group asked: "Can prostate MRI at 3 (tesla) match imaging at 1.5 (tesla) with a (combined endorectal and phased-array coil) in terms of image quality, tumor delineation, and evaluation of the staging criteria, and is it still advantageous to use an endorectal coil?" (AJR, November 2005, Vol. 185:5, pp. 1214-1220).
For their study, they enrolled 24 consecutive patients who were scheduled for radical prostatectomy. The prostate-specific antigen (PSA) levels in these men (mean age of 62 years) ranged from 2-14 ng/mL. Of the 24 patients, all but two underwent surgery.
The first MRI exam was done on a 3-tesla scanner (Signa 3T, GE Healthcare, Chalfont St. Giles, U.K.) using a torso phased-array coil (USA Instruments, Aurora, OH). The second MR scan was done on a 1.5-tesla unit (Magnetom Vision or Symphony, Siemens Medical Solutions, Erlangen, Germany) using an endorectal coil (Medrad, Indianola, PA) and the torso phased-array coil.
 |
| A 62-year-old man with prostate-specific antigen level of 6.3 ng/mL and biopsy-confirmed prostate cancer. Axial (A, above) T2-weighted image acquired with torso phased-array coil at 3 tesla and corresponding image acquired with combined endorectal-body phased-array coil at 1.5 tesla (B, below). |
 |
| Beyersdorff D, Tayamoorian K, Knösel T, Schnorr D, Felix R, Hamm B, Bruhn H, "MRI of Prostate Cancer at 1.5 and 3.0 T: Comparison of Image Quality in Tumor Detection and Staging" (AJR 2005;185:1214-1220). |
The results of preoperative analysis were compared to histology to determine the accuracy of MRI for local staging. Retroanalysis was done to compare the MR images obtained at the two field strengths. Other areas looked at included image quality, the presence of artifacts, periprostatic infiltration, and invasion of adjacent organs.
According to the results, for tumor staging, MRI findings correlated with histopathology in 16 out of 22 cases that underwent prostatectomy. MRI overstaged in four instances and understaged in two. The accuracy of staging on MRI at both field strengths was 73%.
In the retroanalysis, "the images obtained at 1.5 (tesla) were assigned significantly better scores than those obtained at 3 (tesla) for overall image quality and the criteria of delineation of the prostate capsule," the authors wrote.
 |
| Same patient. Coronal (C, above) T2-weighted image acquired with torso phased-array coil at 3 tesla and corresponding image acquired with combined endorectal-body phased-array coil at 1.5 tesla (D, below). |
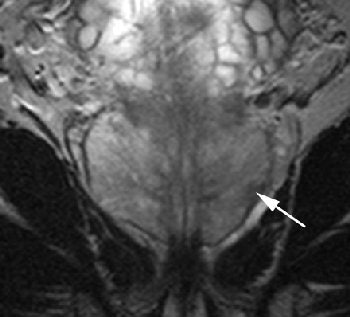 |
| Note hypointense region in peripheral zone of posterolateral aspect in A and C (arrows) and less marked hypointensity on B and D (arrows). Extracapsular extension at either field strength is not seen. Images generated with endorectal coil have better overall image quality. Histology of prostatectomy specimen yielded stage pT2c tumor. |
They also found fewer artifacts on 1.5 tesla with the endorectal coil. The artifacts on 3 tesla were most likely caused by blurring or motion that resulted from the high echo-train length of the MR sequence, the authors explained.
On the images obtained at 1.5 tesla, sensitivity was highest for capsule contiguity, smooth bulging, irregular bulging, direct periprostatic infiltration, and asymmetry of the neurovascular bundle. The latter criteria, along with displacement of the rectoprostatic angle, had higher sensitivity on 3-tesla MR.
"The results of our study suggest that the improvement in the SNR resulting from the higher field strength ... does not reach that achieved with the endorectal coil at 1.5 tesla," the authors stated. However, there was no difference between 1.5 tesla and 3 tesla for tumor staging, they added.
Beyersdorff told AuntMinnie.com that his group has not had a chance to work with prototype 3-tesla endorectal coils that are currently in development. He also said that more sophisticated coils, such as 8-channel phased-array surface coils, would still not be able to approximate the "excellent" SNR ratio achieved with endorectal coils. His group also has not worked with new software that can supposedly negate the need for an endorectal coil during the exam, he added.
However, his group is in the process of developing dedicated sequences, as well as designing their own postprocessing software, for contrast-enhanced MRI of the prostate, Beyersdorff stated.
By Shalmali Pal
AuntMinnie.com staff writer
December 15, 2005
Related Reading
Preop chemoradiotherapy improves local control of rectal cancer, October 19, 2005
3TP debuts prostate MRI software, September 15, 2005
Copyright © 2005 AuntMinnie.com



















