The CT scanner stands behind most, but not all, virtual colonoscopy exams. More than five years ago, researchers led by Dr. Jörg Debatin developed a successful MR colonography (MRC) protocol (Radiology, April 1998, Vol. 207:1 pp. 59-65).
Following the group's success, others have come to value MRI's lack of ionizing radiation and superior soft-tissue resolution in virtual colonoscopy applications. MRC studies, while fewer and smaller than their CT counterparts, have yielded comparable results. Most MRC techniques rely on a gadolinium or barium-enhanced water enema for contrast and colonic distension, while at least one group has successfully used air insufflation as used in CT colonography (AJR, January 2001, Vol. 176:1, pp. 144-146).
In recent efforts to make MR virtual colonoscopy easier for patients, Dr. Thomas Lauenstein, along with Debatin and colleagues from University Hospital in Essen, Germany, have been experimenting with barium fecal-tagging techniques that enable MRC to be performed without purgative bowel cleansing (Topics in Magnetic Resonance Imaging,December 2002, Vol. 13:6, pp. 435-444).
At the 2002 RSNA meeting in Chicago, Lauenstein presented the group's newest study, aimed at optimizing the timing, volume, and protocol used in fecal tagging for MR virtual colonoscopy. The goal is to darken residual stool in the colon to the same MRI signal intensity as the rectal barium enema that is applied before imaging using either air or water, he said. Once the residual fecal material "disappears," the higher-intensity polyps will presumably be easier to detect.
"How do we obviate bowel cleansing? By fecal tagging," Lauenstein said. Taken with regular meals, "the barium agent sticks to the foodstuffs and respectively to the stool in the colon."
The group used two commercial barium-sulfate preparations, Micropaque (1 g barium sulfate per ml; Guerbet, Aulnay-sous-Bois, France), and Maxibar (2.1 g barium sulfate per ml; E-Z-EM, Westbury, NY). Both agents are inexpensive, have a good safety profile, and cause fecal matter to appear so dark as to "disappear" on T1-weighted MR images, Lauenstein said.
The study examined 10 healthy volunteers, each of whom underwent MR virtual colonoscopy (MRC) 10 times, using a slightly different tagging protocol for each exam. A minimum 8-day delay was imposed between scans.
In 10 different protocols, the barium-sulfate dose was varied between 100 ml and 300 ml. The 1-g/ml (Guerbet) agent was alternated with the 2.1-g/ml (E-Z-EM) agent. The number of meals eaten with the tagging agent ranged from four to six. The effect of additional signal-reducing components, iron oxide (500 mg), and lactulose (8 g) was also evaluated.
No spasmolytic agents or intravenous or rectal contrast media were administered. The exam was limited to the evaluation of fecal tagging, and there was no attempt to assess pathology.
After following each prescribed tagging protocol, the subjects underwent MR imaging on a 1.5-tesla Magnetom Sonata (Siemens Medical Solutions, Erlangen Germany) using a T1-weighted 3-D gradient-echo sequence (TR/TE/flip = 1.64/0.6/15).
The researchers measured the signal intensity (SI) of the feces in the ascending, transverse, descending, and sigmoid colon. Average signal-to-noise ratios (SNR) and standard deviations were calculated as parameters for the homogenization of stool signal intensity.
According to the results, each of the tagging protocols lowered signal intensity of the fecal matter significantly compared to no tagging. The Maxibar agent proved superior to Micropaque (p < 0.05). Ingestion of 100 ml was inferior to 200 ml of tagging agent (p < 0.05). There was no benefit from increasing the dose from 200 to 300 ml per meal, or increasing the number of meals from 4 to 6. The ingestion of both lactulose and iron oxide significantly lowered stool signal intensity (p<0.05).
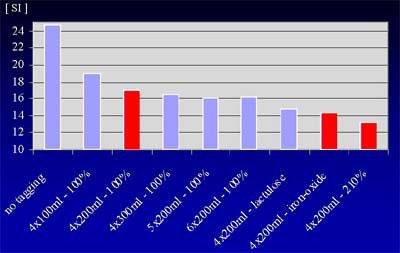 |
| Signal intensity (SI) of fecal material was reduced in response to various tagging protocols. 100% refers to Micropaque formula, which contains 1 g barium-sulfate per ml; 210% refers to Maxibar formula, which contains 2.1 g barium-sulfate per ml. Chart courtesty of Dr. Thomas Lauenstein. |
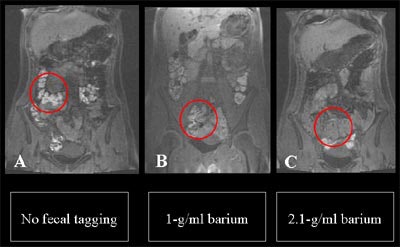 |
| MR colonography without fecal tagging (left) shows higher signal intensity of fecal material compared with image obtained using the 1-g/ml (Micropaque) agent (center). At right, 2.1-g/ml (Maxibar) agent produced the lowest signal intensity. Except for the tagging agent, the protocols (which included four meals without lactulose or iron sulfate) were identical. Images courtesy of Dr. Thomas Lauenstein. |
MR colonography without fecal tagging (left) shows higher signal intensity of fecal material compared with image obtained using the 1-g/ml (Micropaque) agent (center). At right, 2.1-g/ml (Maxibar) agent produced the lowest signal intensity. The protocols, including four meals plus lactulose and iron sulfate, were otherwise identical. Image courtesy of Dr. Thomas Lauenstein.
"The best results were obtained with 200 ml of the high-density (Maxibar) barium sulfate with four meals, plus the additives lactulose (8 g) and iron oxide (500 mg)," Lauenstein concluded. "Due to the focus on their incorporation into adaptive meal preparations, this might even enhance patients’ compliance."
The lactulose and iron oxide have a synergistic effect, he added, because the former is a stool softener while the latter tends to slow down the movement of fecal material through the colon.
By Eric BarnesAuntMinnie.com staff writer
January 22, 2003
Related Reading
Fecal tagging improves detection in virtual colonoscopy, August 29, 2002
In virtual colonoscopy, nothing beats a good prep, July 16, 2002
Prepless virtual colonoscopy shows early promise, June 3, 2002
Copyright © 2003 AuntMinnie.com