FDG-PET scans and memory tests appear to be the best predictors of cognitive problems that may develop into Alzheimer's disease, according to a study published online June 30 in Neurology, the medical journal of the American Academy of Neurology (AAN).
Researchers at the University of California, Berkeley found that the study's 85 patients with mild cognitive impairment (MCI) converted to Alzheimer's disease at an annual rate of 17.2%. The patients with MCI who had abnormal results on both FDG-PET and episodic memory were 11.7 times more likely to convert to Alzheimer's than patients who had normal results on both measures.
The lead author of the study is Susan Landau, PhD, a research scientist with the University of California, Berkeley and Lawrence Berkeley National Laboratory in Berkeley, CA.
ADNI database
Landau and colleagues used data from subjects in the Alzheimer's Disease Neuroimaging Initiative (ADNI), which includes approximately 50 medical centers and universities across the U.S. and Canada. The research project is designed to develop biomarkers of Alzheimer's disease in elderly subjects and validate MRI and PET images, cerebral spinal fluid, and blood biomarkers as predictors of the disease.
As of April 2009, 85 subjects with mild cognitive impairment had baseline data available for all measures of interest for the Berkeley study. Participants were between the ages of 55 and 90 and were followed for an average of 1.9 years.
Clinical diagnostic evaluations were conducted at six, 12, 18, 24, and 36 months. The researchers noted that 61 (72%) of the 85 patients completed five visits (24 months), followed by 13 patients (15%) with four visits (18 months), seven patients with three visits (12 months), and the remaining four patients with six visits (36 months).
The researchers evaluated five factors that have been linked to the development of Alzheimer's disease. Baseline data were obtained for the 85 patients on FDG-PET uptake, apolipoprotein E (APOE) genotypes, cerebrospinal fluid proteins, hippocampus volume, and memory performance.
Alzheimer's detection
The memory test asked each participant to correctly recall a list of words, and blood tests were given to determine the form of the APOE gene, because one form is associated with Alzheimer's disease.
MRI scans were used to measure the size of a subject's hippocampus, which is responsible for learning and memory. Cerebrospinal fluid biomarkers also are known to be useful in predicting Alzheimer's, with the Aβ protein marker indicating amyloid plaque, which disrupts neural connections in the brain.
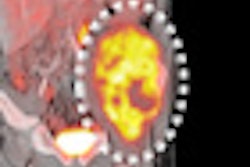
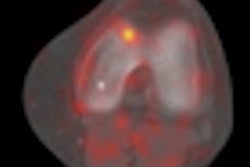
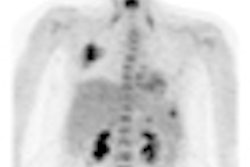
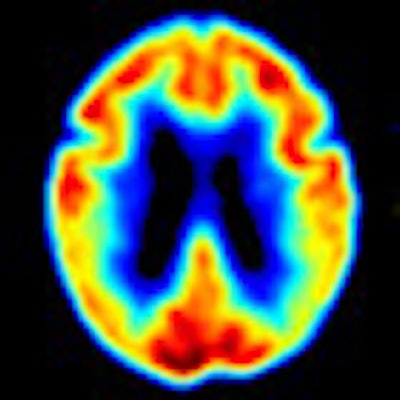
Finally, an FDG-PET brain scan was acquired to detect metabolic abnormalities in the brain that might signal Alzheimer's disease. FDG-PET's glucose metabolism slows when the brain is functioning abnormally, resulting in lower levels of FDG uptake.
"We are inferring that when there is this lowered glucose metabolism in Alzheimer's patients, and even before mild cognitive impairment, the disruption of neural networks is already well under way and that's why we are seeing this global effect," Landau said.
In evaluating the usefulness of the markers to determine whether MCI patients will convert to Alzheimer's, the researchers found that all the measures were useful to some degree. "All the measures did give some information on who will convert or not," Landau added, "but the ones that were most useful were FDG-PET measures and the memory test."
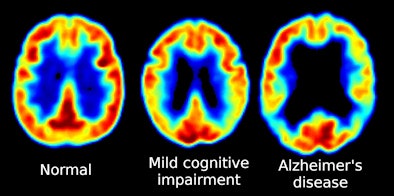 |
| FDG-PET images show reduced glucose metabolism in temporal and parietal regions in patients with MCI and Alzheimer's disease. Images courtesy of Suzanne Baker, PhD; William Jagust, MD; and Susan Landau, PhD. |
Of the 85 MCI participants, 28 (33%, or an annual rate of 17%) converted to Alzheimer's disease. The findings also indicated that the 36 subjects (42%) who expressed Alzheimer's for both FDG-PET and the memory test had an 11.7-fold greater risk of converting to Alzheimer's than subjects who showed no signs of Alzheimer's on both tests.
Subjects who were Alzheimer's-positive on FDG-PET had a 2.72 times greater risk of converting to Alzheimer's than patients who were Alzheimer's-negative on FDG-PET.
Because people with mild cognitive impairment decline at different rates and some never develop Alzheimer's, there is a need for tools that can better predict who might benefit most from treatment, Landau noted.
"The current clinical role of these and other biomarkers in dementia care is relatively limited, largely because of the lack of effective treatment," the authors also wrote. "However, our results suggest that these biomarkers could be effective in identifying patients with MCI who are more likely to progress to [Alzheimer's] over relatively brief time periods. This approach could be useful for identifying patients who would benefit from treatment when it becomes available and for selecting subjects in clinical trials of therapeutic agents for MCI."
The study was supported by the National Institutes of Health (NIH) and the Dana Foundation.
By Wayne Forrest
AuntMinnie.com staff writer
June 30, 2010
Related Reading
MRI finds genetic link in Alzheimer's disease, June 14, 2010
PET can help clarify dementia diagnoses, May 3, 2010
MRI hippocampal measurement doesn't predict cognitive decline, April 26, 2010
PET finds risk factor for Alzheimer's in Latinos, April 15, 2010
MR scans may detect signs of early dementia in elderly, April 14, 2010
Copyright © 2010 AuntMinnie.com